Merck Lowered the Price of Januvia—Insurers Dropped It from Formularies [News Roundup]
Merck Lowered the Price of Januvia—Insurers Dropped It from Formularies and other notes from around the interweb:
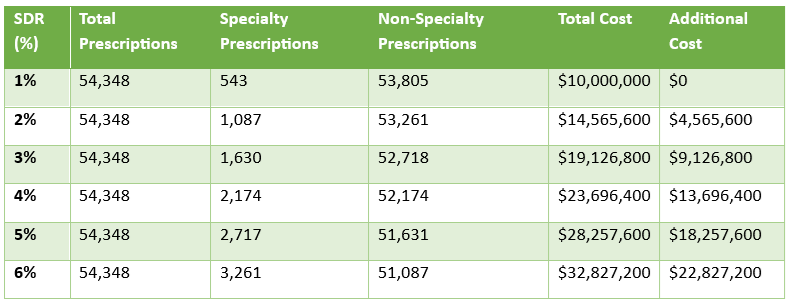
- Merck Lowered the Price of Januvia—Insurers Dropped It from Formularies. In a move that should have been great news for patients, Merck significantly reduced the price of its blockbuster diabetes drug, Januvia (sitagliptin). However, instead of benefiting from the savings, many insured patients are discovering that their insurance plans no longer cover it. The culprit? Pharmacy Benefit Managers (PBMs)—powerful intermediaries that negotiate drug prices on behalf of insurance companies—have removed Januvia from their formularies. Those same powerful intermediaries are the latest in the hot seat for their predatory behavior in the United States health system. PBMs have been found to make coverage decisions based on their financial incentives rather than patient access to affordable medication.
- Walgreens Goes From $100 Billion Health Giant to Private-Equity Salvage Project. Customers bought more household items online at sites such as Amazon.com, instead of Walgreens’s more than 8,000 stores across the U.S. The pharmacy chain inked deals with other drug suppliers and doctors’ offices, but stood pat while rivals, including CVS and Express Scripts, merged with big health insurers, gaining control of the medical-reimbursement purse strings that were squeezing pharmacies. Walgreens cash flow sagged, its debt piled up and shares sank. And on Thursday, Walgreens was sold to private-equity firm Sycamore for $10 billion, down a staggering 91% from its $106 billion peak in 2015. The storied pharmacy chain—which became a ubiquitous seller of everything from diabetes injections to nail files as retailers consolidated across the U.S.—fell after it neglected to keep up with customer preference to buy online and failed to navigate the fierce competition and intense cost pressures of healthcare.
- The Endless Opportunities ChatGPT Creates for Pharmacists. With the recent rise of artificial intelligence (AI), not only in the pharmacy but across society, major players within the AI space have designed technology possible for any human being to adapt. One of the most notable examples is ChatGPT, an AI language model capable of answering straightforward questions with detailed answers. “ChatGPT is an AI language model capable of responding in straightforward language to medication-related questions,” wrote authors of a study published in the Journal of the American Pharmacists Association (JAPhA). “ChatGPT may assist clinicians in analyzing clinical cases and become a potential tool for supporting pharmacists in providing medication therapy management (MTM) and other health services.”
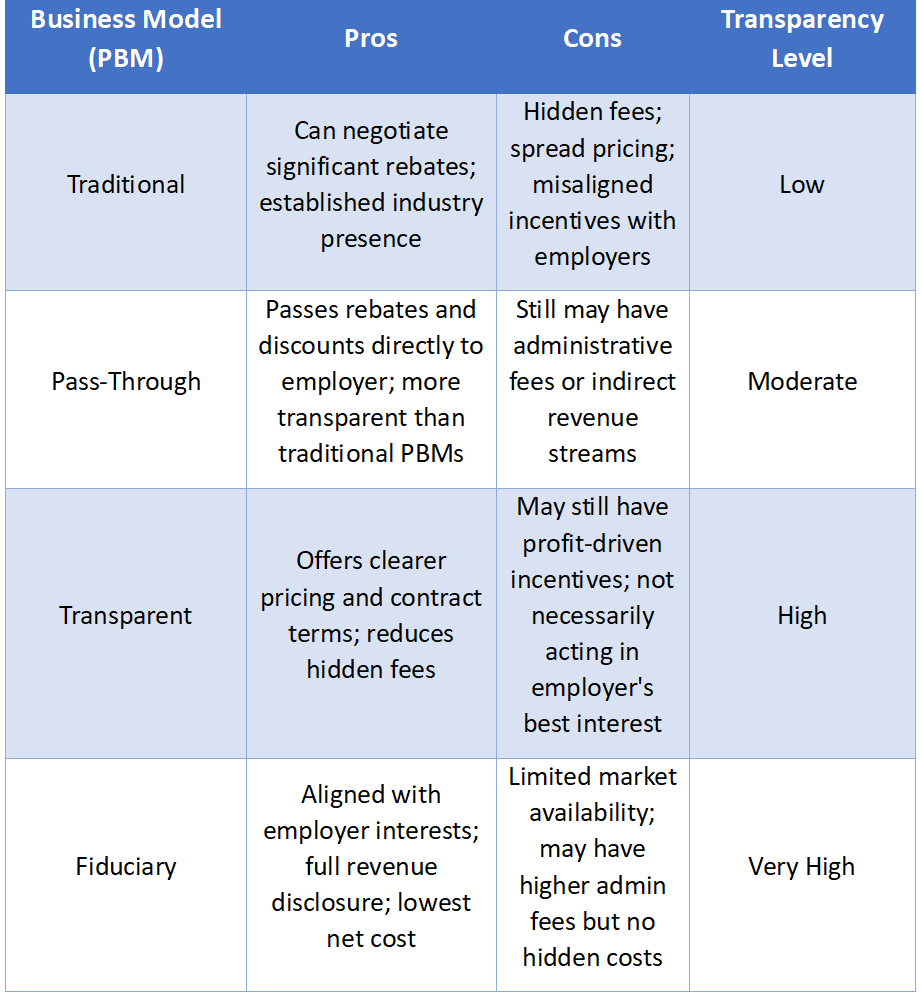
- PBM Reform: Tackling Transparency, Pricing, and Patient Access. Pharmacy benefit manager (PBM) reform has become a substantial topic of debate for the past decades as patients and health care providers advocate for improved transparency, fair pricing, and better access to critical therapies. PBMs occupy a central role in the drug price supply chain, acting as intermediaries between drug companies, insurers, and pharmacies to determine which drugs will be most available and what they will cost. The top 3 PBMs control 80% of the national market, giving them significant power to negotiate drug prices and rebates, create formularies, determine which pharmacies patients can use, process prescription drug claims, and set reimbursement rates for pharmacies. However, there is a significant lack of transparency around how these costs are negotiated between health plans and pharmaceutical manufacturers, leading to calls for policy reform.
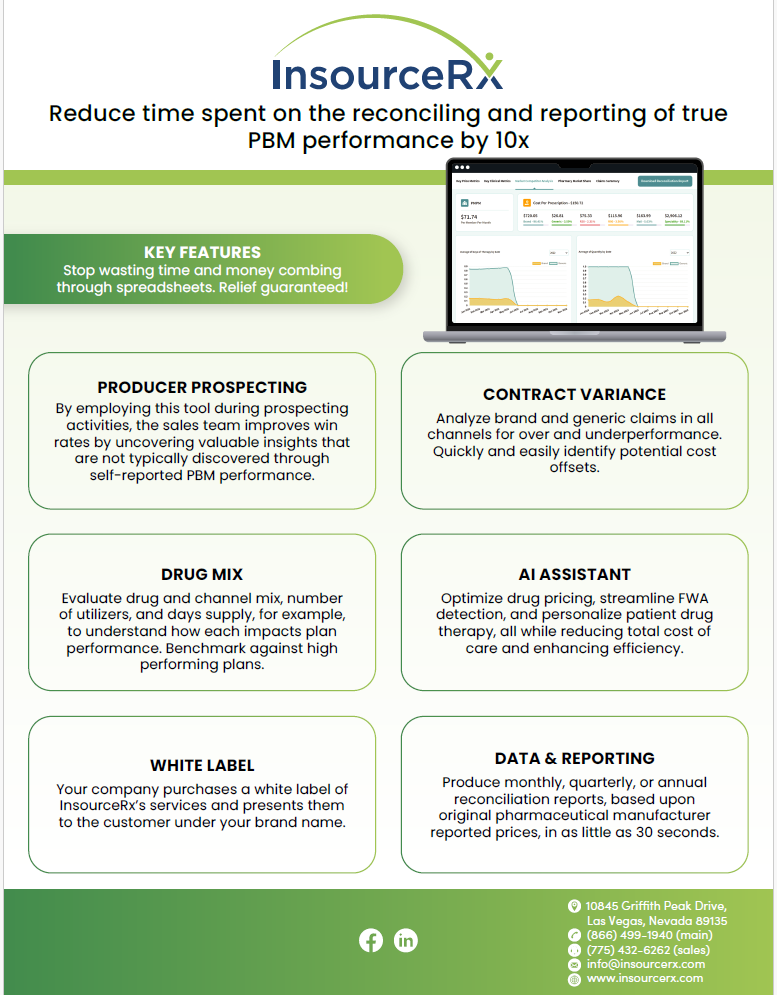
Why TransparentRx Is Your Trusted Partner for Smarter Pharmacy Benefits
At TransparentRx, we specialize in delivering fiduciary pharmacy benefit management services that prioritize transparency, cost containment, and optimal patient outcomes. Our unique approach helps self-funded employers, benefits consultants, and health plan sponsors navigate the complexities of pharmacy benefits while reducing costs and enhancing care.
If you’re ready to take control of your pharmacy benefit strategy and eliminate hidden fees, contact TransparentRx today for a consultation. Let us help you achieve smarter, more effective benefits management.