In my Certified Pharmacy Benefits Specialist course, I can count on one thing happening during each term. When the topic of DAW or dispense as written codes is covered it stirs up some serious emotions in retail pharmacists. A pharmacist might take the floor and talk for 10 minutes about how the DAW 9 code is being used. It ticks them off and rightfully so.
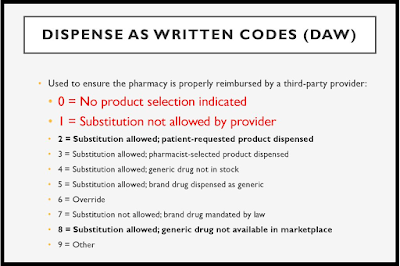
DAW codes are important in billing claims correctly to a patient’s insurance plan. DAW codes are used by insurance companies and PBMs to help determine the reimbursement to the pharmacy and if the medication is eligible for full or partial coverage. Claims must be billed/filed correctly so that patients receive the appropriate drug products at the correct price. DAW 0 is used most of the time while DAW 1 is used sparingly. DAW 9 is increasingly becoming popular and being put into place by PBMs.
For most plan sponsors, brokers and consultants the use of DAW 9 goes unnoticed in how it increases cost and wasteful spending. Typically, a generic drug has been dispensed because it is a less costly alternative when compared to the brand name product. In short, when prescribers write a prescription and sign Product Substitution Permitted — the pharmacist must dispense the brand name product for the product to be covered by the patient’s insurance. This is done by changing the computer DAW code from a 0 to a 9.
In a retail pharmacy, it is the pharmacy technician who most often gets the claim paid. So when a claim is rejected with a DAW 0 code the pharmacy technician simply cycles through all the DAW codes until one is accepted. You may be asking, “why would a PBM engage in this practice?” In a word – REBATES! If you’ve taken a deal with a non-fiduciary PBM which calls for a $0 admin fee on the pharmacy benefit or you’ve decided to forgo rebates in lieu of admin fee credits on the medical benefit, how else do you expect the PBM to make money?
Artificially low admin fees on the pharmacy benefit and/or forgoing rebates for admin fee credits on the medical benefit gives a PBM the green light to employ hidden cash flow tactics, like DAW 9, to augment their service fee. In the case of DAW 9, that augmentation occurs in the non-fiduciary PBMs share of manufacturer revenues (rebates). In 2020, you can’t be doing business with a PBM that doesn’t provide radical transparency. It’s fiscally irresponsible. Unfortunately, most plan sponsors don’t know what they don’t know.