CVS Caremark, with the same parent company as CVS retail pharmacies, manages pharmacy benefits for four of the five Medicaid managed care companies. Last year it kept 8.7 percent or the payments it received, or $197.3 million. OptumRx does work for the other insurer and kept 9.4 percent, or $26.4 million.
Tyrone’s Commentary:
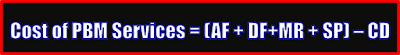
Finally, someone is tackling a critical issue that too often gets tabled. I’ve been trying to bring PBM service fees (watch video below) to the mainstream for six years! The one question I have is why are public sector managers leading the charge?
 |
| 6-Minute Video: Click to Learn More |
I don’t know the answer to that question but I do know the public sector is better at managing pharmacy costs than are commercial payers and that my loyal readers is a problem. Worst case scenario, it may very well be a dereliction of fiduciary duty by CFOs and HR Execs.
Greg Moody, the director of the Ohio Department of Health Transformation, which oversees Ohio Medicaid, said Ohio needs more information before it determines what is a fair share for the pharmacy benefit managers.
“At this stage we’re not saying that’s too high or too low,” Moody said. “What we’re saying is this is information we’ve never had before. And now the state, the managed care plans, the pharmacies have more information to make their argument and determine if that number is too high or too low or what should happen next.”