Blue Cross Blue Shield insurers in six states have sued CVS Health Corp. over an alleged scheme to overcharge them for generic drugs by submitting claims for payment at “inflated prices.” The lawsuit, filed May 27 in the Rhode Island federal court, added to mounting pressure that CVS has been facing since 2015 over its cash discount programs, which it said were designed to compete with Walmart and other “big-box” discounted pharmacies.
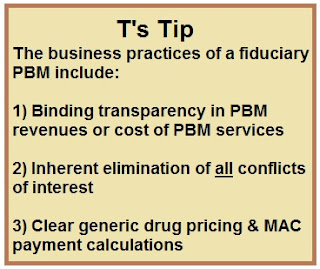
Tyrone’s Commentary:
Derica Rice was Executive Vice President of CVS Health and President of CVS Caremark, the pharmacy benefits management business of CVS Health, from March 2018 through February 2020. Prior to that time, he was employed in various executive positions at Eli Lilly and Company since 1990, most recently serving as Executive Vice President of Global Services and Chief Financial Officer from 2006 to 2017. In less than two years he quietly departed CVS, why? My guess is that due to his pharmaceutical manufacturer and finance background he and the senior leadership team at CVS didn’t see eye to eye on things such as transparency.
According to the complaint, health insurers typically negotiate “lesser-of” contracts with pharmacy benefits middlemen to pay the lower cost of either the negotiated drug price or the cash price that insured patients would pay. But the BCBS companies alleged that CVS had offered lower prices for “hundreds” of generic drugs and later told insurers that the prices were much higher than they actually were.
“By intentionally submitting falsely inflated usual and customary prices, CVS knew that it was being overpaid for these generic drug transactions. In fact, as internal documents show, that was CVS’s plan all along,” BCBS’s attorneys from Partridge Snow & Hahn wrote in the 46-page complaint.