The debate on whether the Big 3 Pharmacy Benefit Managers (PBMs) offer better price savings just because of their size is a myth. The notion is largely perpetuated by the old guard who has benefited from overpayments received from opaque PBM business practices. However, the truth is that the Big 3 have more purchasing power, but their clients often don’t realize the full benefit. Does size really matter when it comes to pharmacy benefit managers and cost savings?
PBMs generate revenue from rebates following each eligible drug claim. Therefore, a PBM’s interest typically rests in raising prescription drug prices rather than decreasing them to get larger rebates. Pharmaceutical firms’ priorities have been fundamentally altered by this method; rather than competing to provide patients with high-quality, reasonably priced medications, they are now more interested in gaining the PBMs’ support for the top spot on formularies by providing generous incentives thus driving up costs.
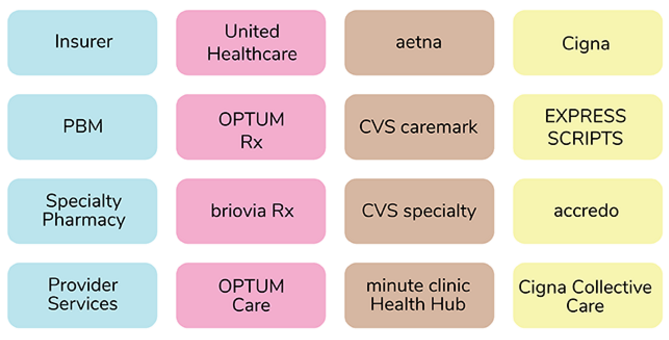
Furthermore, there is a high concentration of purchasing power due to the vertical integration of the major PBMs, specialty pharmacies, and insurers. As a result, the three largest PBMs control 80% of the market for prescription volume. The following diagram shows the vertical business connections between retail chains, PBMs, and insurers:
For instance, while a rebate aggregator may pay a $3000 rebate for drug “A” and return every penny back to the client with an audit trail, the Big 3 may earn $4000 on the same drug but retain $1200 in-house, resulting in the plan sponsor pocketing an additional $200 when working with a radically transparent, albeit smaller, PBM.
Additionally, non-fiduciary PBMs use estimates in their price quotes, which can lead to discrepancies between projected and actual costs. As a result, the plan sponsor’s PBM contract is the most valuable tool to address the actual level of drug spending, not cost projections. However, non-fiduciary PBMs often use opaque contract language to eat away at the proposed savings, such as discount and rebate guarantees as soon as your plan goes live.
It’s essential to consider the PBM management fee in how you procure pharmacy benefit management services. The PBM management fee is largely an undisclosed fee that non-fiduciary PBMs charge for providing their services to plan sponsors, and the bulk of this fee is buried in the final plan pharmacy cost. Therefore, the contract is king.
Check out this free webinar if you’ve never considered the PBM management fee in PBM procurement. With transparency in PBM practices, smaller PBMs can offer more significant cost savings, as illustrated in the webinar below:
Remember that the size of a PBM does not always guarantee better price savings. Look for transparency in PBM practices to ensure that you’re getting the most value out of your pharmacy benefit management services. Having a trained eye enables a person to quickly and accurately identify details, patterns, and anomalies that may not be immediately apparent to an untrained observer. This can lead to better decision-making, problem-solving, and overall performance in managing a pharmacy benefit. The Certified Pharmacy Benefits Specialist (CPBS) program is the #1 training option for employee benefit brokers, consultants, HR, and Finance.