 |
| Source: International Federation Employee Benefit Plans |
Starting Jan. 1, BlueCross BlueShield of Tennessee will stop reimbursing providers for certain specialty drugs typically administered in a doctor’s office or hospital setting. These expensive medications are used to treat conditions ranging from autoimmune disorders — such as rheumatoid arthritis, Crohn’s disease and ulcerative colitis — to some types of cancer and eye conditions. The change doesn’t affect drugs patients inject or take on their own.
Tyrone’s Commentary:
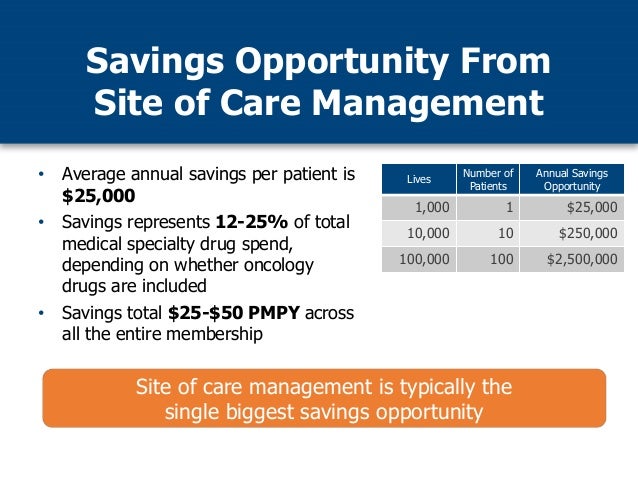
Site of care optimization simply means having a strategy to seek out and promote the most economical and clinically effective place to deliver care for a particular patient. While this may prove bothersome to some patients and physicians, you can’t have it both ways. Whomever covers the largest share of the drug cost should have the most say so in the locations from which these drugs are dispensed (as long as the decision doesn’t risk the patient’s safety or outcomes). Site of care management is good for self-funded employers. Since they cover most of the drug costs, its only right these employers have the final say so in where high cost drugs are dispensed. I don’t walk into my friends’ homes go into the refrigerator and put my feet on their sofas. You know why? I don’t pay their mortgages.
Providers will instead be required to obtain those drugs through a specialty pharmacy in BlueCross BlueShield’s preferred network. The move is the insurer’s attempt to slow the skyrocketing cost of specialty pharmaceuticals, which account for only 1% of prescriptions but almost half of the company’s prescription costs, according to company spokesman Roy Vaughn.