Generic Substitution Rate (GSR) and employer-sponsored prescription drug costs go together like peanut butter and jelly or Glory green beans and meatloaf. If you’ve never tried Glory green beans pick up a couple of cans during your next trip to the supermarket. You will ditch Green Giant or Del Monte and never go back. Thank me later.
It is clear that every pharmacy benefit manager offers clinical services. These clinical services include but are not limited to formulary management and drug utilization management. Drug utilization management includes services such as prior authorization, step therapy, quantity limits, therapeutic substitution, dose optimization, refill to soon, and a host of others. What isn’t so clear is how does a self-insured employer or broker measure the performance of clinical services? Generic Substitution Rate (GSR) is the best metric for measuring PBM clinical management performance.
Clinical services are popular among purchasers of PBM services, yet their effectiveness remains a mystery to many. Let’s first review the Big Three for drug utilization management programs before diving into GSR and its significance. The Big Three includes prior authorization, quantity limits and step therapy services.
Prior Authorization (PA). Requires approval by the PBM or plan administrator before payment to the pharmacy is permitted. The drugs which require prior authorization or PA are high cost, have the potential for abuse or waste, or require monitoring to reduce the risk for dangerous side effects.
Quantity Limits (QL). A maximum quantity of drugs that can be dispensed to a patient at one time. The primary purpose of quantity limits is to reduce wasteful spending in the case a 90-day supply isn’t necessary, for instance. All specialty drugs should have a 30-day or less supply quantity limit.
Step Therapy (ST). Costly drugs are dispensed only when the patient has tried a less costly drug. For example, a lower cost specialty or non-specialty drug would be required before the more costly specialty drug is approved by the PBM or plan administrator. Some benefit designs may require failure on two or more drugs in a step therapy process before the costliest drug is approved.
I’m occasionally asked by brokers and plan administrators, “should we be tracking our Generic Substitution Rate?” My answer is always the same, an emphatic yes! Generic Dispense Rate (GDR) and Generic Substitution Rate are major contributors to PMPM plan cost. In fact, GDR and GSR are congruent. Because they work in harmony, high performance with GDR means the same for GSR and vice versa. GDR and GSR as major contributors to final plan costs is an understatement.
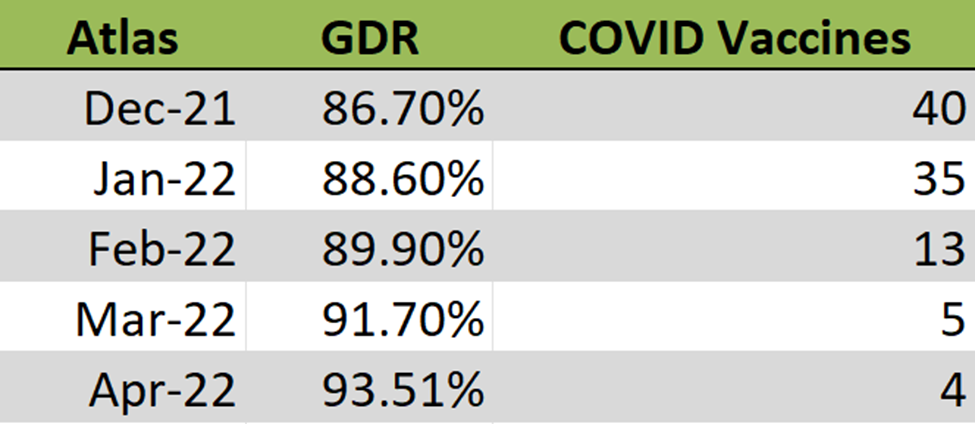
Figure 1 is the actual Generic Dispense Rate (GDR) performance from one of our clients. Generic Dispense Rate (GDR) is the percentage of all prescription drug fills that were for generics. For April, this client’s GDR was 93.5%. For every 1% increase in GDR a plan can expect to realize a 2.5% reduction in gross drug spend. Going from an 80% to 90% GDR means a $500K savings for a plan with a $2M annual drug spend, for example.
The Generic Substitution Rate (GSR) is the rate at which generic drugs are dispensed in place of their brand reference products. The Generic Substitution Rate (GSR) for this client (Figure 1) is 99.3%. In layman’s terms, a generic drug is dispensed in place of its brand reference product more than 99% of the time! If a PBM is managing its clinical programs efficiently, your GDR should be right at or above 90% and the GSR above 95%. A high GSR, 95% or above, is a clear indicator whether drug utilization management programs are being run efficiently or are just being rubberstamped.
Generic Substitution Rate = number of generic drug claims/sum of generic and MSB drug claims
A 2020 analysis from Avalere Health finds 52% of Part D plans achieve generic substitution rates above 75%. Put another way, 48% of Part D plans were unable to achieve generic substitution rates above 75%. This is horrifying as far as wastefulness. In a 2019 report, IQVIA Institute estimates generics make up 90% of all prescriptions but they are only a fraction of overall costs. Brand-name drugs make up the remaining 10% but account for 79% of all drug spending. An 80% GDR is not good, it is a clear-cut indicator of poor clinical management whether you care or not.
Generic Substitution Rate Conclusion
Non-fiduciary PBMs have little incentive to help plan sponsors monitor the GSR metric. Simply put, they don’t want to be deemed as fiduciaries by guiding you in the right direction and identifying problem areas. Ask your PBM’s executive sponsor, not the sales executive, are you contractually obligated to help contain our costs? 50% of PBMs will say no, 40% will be unsure, 10% will say yes but 90% of the 10% that say yes will be disingenuous. That leaves 1 out every 100 PBMs who have contractually obligated themselves to contain your costs. TransparentRx is part of the 99th percentile so click here to learn more about us.