Since open communication is essential in the partnership between pharmacy benefit managers (PBM) and unions, health plans, health systems, commercial and public sector employers, you should be able to ask tough questions of prospective PBMs before selecting one. Ask PBMs these 8 questions as you look for the right fit for your company.
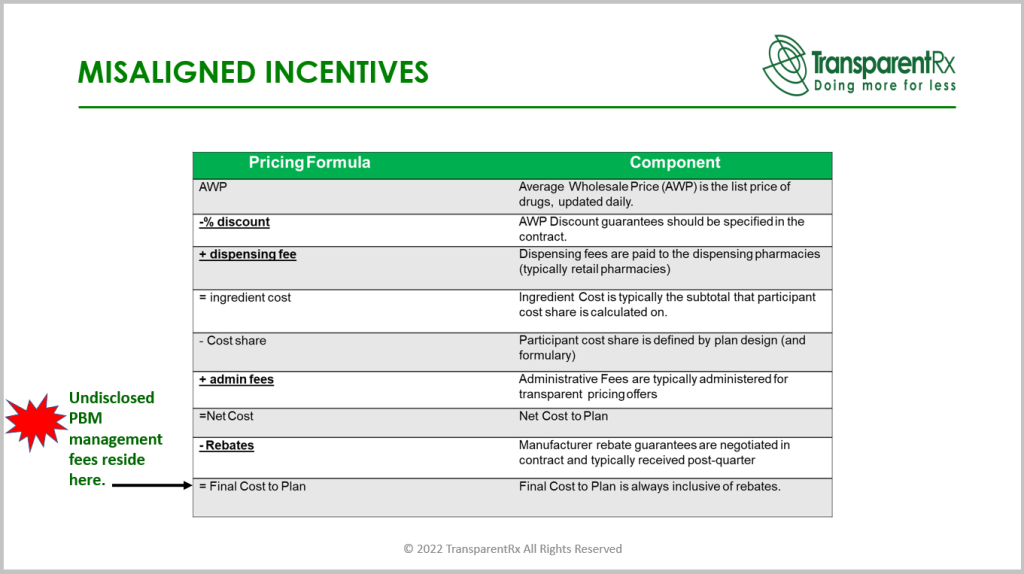
- What will be your earnings after cash disbursements (EACD)? The amount of money a PBM receives in exchange for the services it provides to your organization is referred to as EACD, or earnings after cash disbursements. You can only begin to comprehend the magnitude of overpayments after discovering how much money a non-fiduciary PBM retains for itself. The ingenious of EACD is that it is hidden in your plan’s final cost! One may fairly conclude that the $25 PMPM cost discrepancy between PBMs “A” and “B” who each offer yearly costs of $63 and $88 PMPM, respectively, represents revenue for the PBM. A commercial employer with 8000 members contributes an additional $2.4 million yearly to its cost for PBM “B” management fees! The management fee or EACD of the PBM must be understood and incorporated into your financial analysis. Both the quantity and the source of the PBM’s money flows must be open to disclosure.
- What is Your Book GDR, or Generic Dispensing Ratio? Verify that your PBM is not a member of any brand-specific incentive programs. The adoption of generic substitutes is discouraged by brand-name incentive schemes, which push PBMs to settle more prescriptions for name-brand medications. These could prompt them to suggest pricier, name-brand drugs. The fact that generic medications are less expensive means you want a PBM that supports them. That can help you find less expensive options, which can save you money. GDR is the proportion of prescription drug claims that are generic. The generic dispensing ratio, or GDR, is 82% if there are 82 generic claims out of 100 total claims. Data from HealthPartners show that a 1% increase in generic drug use might result in a 5% reduction in pharmacy expenses. Goal ≥ 90%.
- What is Your Book PDC, or Proportion of Days Covered? By examining the percentage of days that a person has access to the drug throughout a certain period of interest, the proportion of days covered (PDC) is used to evaluate medication adherence. For instance, from January 1 and December 31, “Amy” fills a prescription for 30 pills 11 times. January 9 saw the initial fill. This covers 330 of the 356 days between January 9 and December 31 that were covered by refills. Consequently, 93% of days are covered. Poor medication adherence leads to higher medical costs and wasteful drug spending. Goal ≥ 80%.
- What is Your Book PMPM Cost? Pharmacy benefits administration revolves upon one unchangeable fact. For unions, health plans, health systems, commercial and public sector employers, the most crucial financial statistic in pharmacy benefits administration is the PMPM or per member per month cost. Do you ask why? PMPM considers all costs, including but not restricted to ingredient costs, clinical performance when product mix and utilization are the primary cost drivers, rebates, and ancillary expenditures like PAs, UMs, or manufacturer assistance programs as well as the PBM management charge!
- Will You Ensure Accessibility to Independent Pharmacies? If your pharmacy benefit management company also operates a pharmacy, there can be a conflict of interest. They shouldn’t have carte blanche on the formulary, network makeup or even drug utilization management programs. Make sure to request a report every month outlining pharmacy performance when you want to deal with a PBM that has its own pharmacy. You should also insist that they seek your approval before prescribing high-cost specialty drugs.
- Use Acquisition-Based Pricing in Your Business? A spread is the difference in the amount reimbursed to pharmacies and subsequently billed to commercial employers for the exact claim. With that said, price benchmarks (i.e., AWP, MAC, NADAC etc.) are irrelevant when the PBM doesn’t take a spread. There is a floor in the reimbursement pharmacies will accept from PBMs. Acquisition-based pricing in pharmacy benefits means the PBM bills its clients exactly what it paid out for ingredient cost. Look for a PBM that contractually prohibits itself from profiting from spreads which increases their profits through hidden cash flow streams. By doing that, you can end up saving money over time.
- Do You Allow 90-Day Maintenance Networks? The adherence rates and discounts at mail-order pharmacies are often higher. The risks of auto-refill programs and increased out-of-pocket expenditures for medications sometimes outweigh the benefits, causing consumers to hoard prescriptions they don’t need. A mail-order pharmacy can be replaced with a 90-day maintenance network from a retail pharmacy, which will eliminate these problems and permit patients to communicate with pharmacists directly.
- What Kind of Education Can You Provide Employees? To help employees realize which pharmacies give the most value to the business, your PBM should offer educational programs. For instance, employees have more affordable alternatives at Costco and Walmart pharmacies than at other major pharmacy stores. By providing the same drugs for less money, they may deliver greater value. You can help your business save money by training your personnel.
Find a PBM you can trust if you want to save on your pharmacy costs. Find someone who can satisfy your needs and offer radical transparency to do that. Spend some time obtaining the responses to these questions before evaluating your PBM possibilities. Then, select the company that can meet both your demands and the greatest arrangement for you. Ask PBMs these 8 questions to save money and ensure that you are happy with the service they provide.