 |
| Radical transparency in pharmacy benefits management starts with training and education. Click here to begin yours. |
For years, Frahm’s South Side Drug bought pills from distributors, and dispensed prescriptions to the Wapello County jail. In turn, the pharmacy got reimbursed for the drugs by CVS Health Corp., which managed the county’s drug benefits plan.
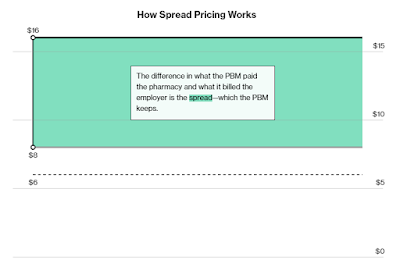
As he compared the newspaper notice with his own records, and then with the county’s, Frahm saw that for a bottle of generic antipsychotic pills, CVS had billed Wapello County $198.22. But South Side Drug was reimbursed just $5.73.
So why was CVS charging almost $200 for a bottle of pills that it told the pharmacy was worth less than $6? And what was the company doing with the other $192.49?
Tyrone’s Commentary:
It’s not a secret at least for those who regularly read this blog or follow me on LinkedIn.
Frahm had stumbled across what’s known as spread pricing, where companies like CVS mark up—sometimes dramatically—the difference between the amount they reimburse pharmacies for a drug and the amount they charge their clients.