 |
| Click to Enlarge |
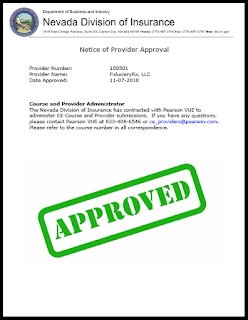
This achievement is bittersweet so allow me to provide the back story. Approximately four years ago, we applied to the Nevada Division of Insurance, our home state, to become a continuing education service provider.
A primary benefit of being certified in our home state is reciprocity. This means approval by our home state would be recognized by every other state in the country without having to go through the full application process within those states. Reciprocity reduces cost and significantly reduces the administrative burden. We assumed getting approved as a CE (continuing education) provider in the same state for which we are domiciled was a no-brainer until it wasn’t!
Because the state of Nevada didn’t regulate PBMs, TransparentRx’s initial application to become a CE provider was not approved. Those of you familiar with these sorts of applications know that you can’t just try once and give up. You must push through and sometimes that requires educating or partnering with the entity who has the final say so.
It just didn’t make sense to us other states approved us who didn’t regulate PBMs so why Nevada. It turns out Nevada was just an anomaly. Consequently, we petitioned the Nevada Division of Insurance for two years and finally last week we were approved as a CE provider. As a result, our approval is now recognized by the remaining 49 states without having to go through the full application process with each individual state. Can I get an amen?
Imagine having to submit an application, renew each course and/or each instructor for all 50 states each having their own applications, deadlines, costs etc. This was a monumental task which has finally been lifted. I’m grateful but…
There is always a but isn’t there? The but in this case is that the state of Nevada is now going to regulate pharmacy benefit managers. Good, bad or indifferent I’ve always preferred a laissez-faire approach to policy when it comes to the free market.
Coincidentally, the state of California just passed Assembly Bill 315 which was written to secure more disclosure and transparency from PBMs. This is extremely significant legislation. Since California usually takes the lead on policy and regulation, expect more states to follow their lead.
Click here to view Assembly Bill 315 in its entirety.