A study exploring Florida’s prescription drug costs through the Medicaid program found that pharmacy benefit managers (PBMs) profited $89 million dollars, mostly from a spread pricing contract scheme that charges the state higher cost than will be disbursed to the pharmacist.
 |
| Click to Learn More |
Florida’s Medicaid program is contracted out to private healthcare companies like CVS Caremark, Humana, etc. Those private companies then take Medicaid dollars and draw up contracts with pharmacies around the state. PBMs play the role of negotiating drug prices between pharmacy suppliers and payers; they have an outsize stake in what consumers pay for their prescription drugs.
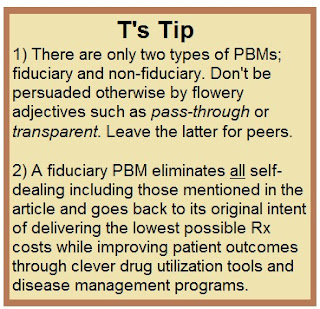
PBMs in Florida operate in 2 ways depending on the county – pass-through or spread. Pass-through pricing reimburses pharmacists the cost of the drug, while PBMs take a small fee. Spread, on the other hand, reimburses a pharmacy a different amount for the drugs than what it charges the state. Kevin Duane of SPAR (Small business Pharmacies Aligned for Reform) who finds it “indefensible” that the PBMs under pass-through contracts filled 2 million more prescriptions and made tens of millions of dollars less than those under spread contracts.
Commissioned by the state Agency for Healthcare Administration (AHCA), the study found that spread pricing contracts pay pharmacists less in reimbursement and keep, on average, 9.5% of the transaction, whereas pass-through models take a $1.45 administration fee and reimburse pharmacists the full cost.