A self-insured employer gets hit with $50 million in claims for just two members and wants the stop loss carrier and PBM to pay up. When pharmacy benefits are loosely managed, self-insured employers play right into the hands of drugmakers, rebate aggregators, non-fiduciary PBMs, and specialty pharmacies who all stand to benefit financially. Micromanaging a pharmacy benefit can nonetheless lead to very satisfied participants and improved medical outcomes.
Micromanagement refers to a management style where a manager closely observes and controls the work of their employees, often involving themselves in every aspect of their work. Micromanagers tend to be excessively controlling and directive, often providing constant feedback and criticism.
Advantages of micromanagement:
- Helps ensure that work is being done correctly and efficiently
- Allows for immediate correction of mistakes or problems
- Provides a high level of detail and precision in the work being done
- Can be useful in situations where there is a high level of risk or complexity
Disadvantages of micromanagement:
- Can create a negative work environment, leading to demotivated PBM employees and high turnover rates
- Can lead to a lack of creativity and innovation, as PBM employees may feel discouraged from taking risks or trying new things
- Can be time-consuming and create unnecessary work for the PBM
- Can limit the development of employee skills and independence, as they may become overly reliant on the broker’s or consultant’s guidance.
Overall, while micromanagement can have some benefits in certain situations, it is generally not considered an effective workplace management style as it can lead to a range of negative consequences for both employees and the organization as a whole. A more hands-off approach that focuses on trust, collaboration, and empowerment tends to be more effective in promoting a positive work culture and achieving long-term success.
However, in pharmacy benefits management, micromanagement is the rule not the exception. Loose management of the pharmacy benefit is all fine and dandy until a self-insured employer gets hit with $50 million in claims for just two members. Poor utilization management by PBMs doesn’t show up in RFPs even though it is a major cost driver.
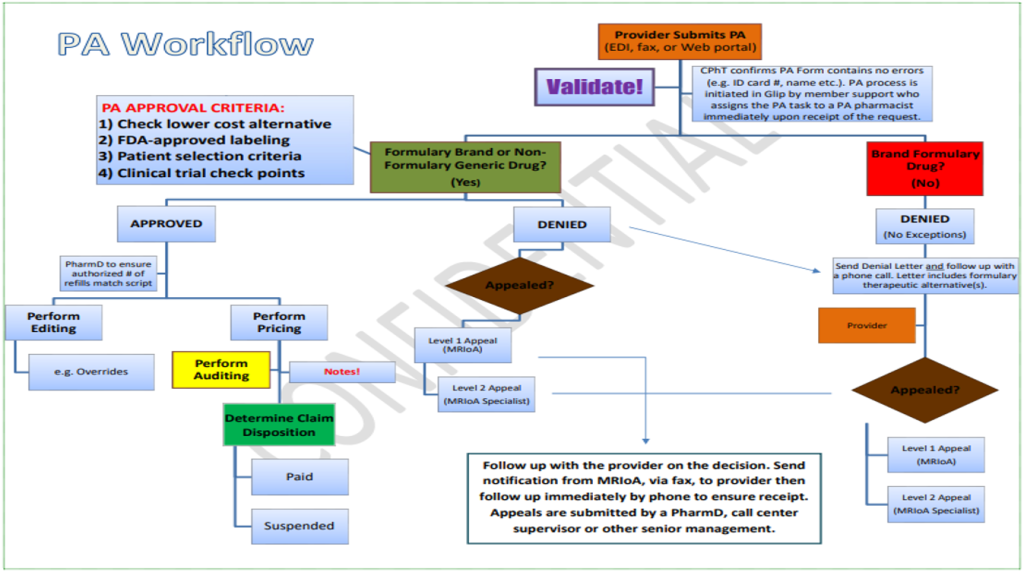
The claims in question herein would have never made it through the TransparentRx clinical review process. Few PBMs in their PA workflow adhere to FDA-approved labeling, patient selection criteria, and clinical trial check points. Micromanagement of the pharmacy benefit acts as a de facto insurance policy.