Biosimilars Are Mighty, Can Help Alleviate Drug Spend Cost Burden and other notes from around the interweb:
- Ohio attorney general sues pharmacy benefit managers, calling them gangsters. Calling them “modern gangsters,” Ohio Attorney General Dave Yost on Monday accused pharmacy benefit managers of illegally driving up drug prices for patients who rely on insulin and other key medications. “Medications shouldn’t cost an arm and a leg, metaphorically or literally,” Yost said in a written statement. “Insulin is just a symptom of the problem; PBMs are the disease.” Yost filed a lawsuit in Delaware County Common Pleas Court against Express Scripts, Prime Therapeutics, Ascent, Humana Pharmacy Solutions and two parent companies. He alleges the companies colluded to control drug prices and have failed to live up to promises to negotiate lower drug prices from manufacturers and deliver those savings to patients. Instead, Express Scripts created a complex ‘pay to play’ rebate scheme that pushes manufacturers to boost drug prices to get their medications on preferred lists.
- Pharmacy Benefit Manager Transparency Act Passes in Senate Committee Vote. On March 22, 2023, the Senate Committee on Commerce, Science and Transportation voted 18-9 to approve sending the bipartisan Pharmacy Benefit Manager (PBM) Transparency Act to the full Senate. The bill introduced by Democrat Commerce Committee Chair Senator Maria Cantwell of Washington and Republican Budget Committee Ranking Member Senator Chuck Grassley of Iowa in January 2023 aims to make prescription drug pricing more transparent. The Congressional Budget Office’s preliminary estimates suggest that the PBM Transparency Act would save $740 million to taxpayers over the next 10 years. The legislation arises out of substantial concerns about the anti-competitive and predatory tactics that PBMs have engaged in throughout the past decade to erode the prevalence of independent pharmacies across the country.
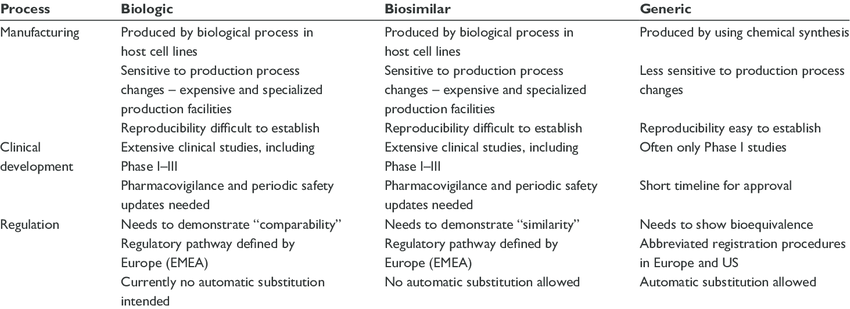
- Biosimilars Are Mighty, Can Help Alleviate Drug Spend Cost Burden. Biosimilar availability also lends itself to more opportunities for substitution at the pharmacy level, like how generic products are substituted for brand name medications. However, for one biosimilar to be substituted for another without requiring physician permission, it must have an interchangeability designation from the FDA. To obtain interchangeability, most products, excluding insulins and ophthalmology products, companies are required to conduct additional clinical trials—after which pharmacists can automatically substitute them for the reference product, provided state laws allow it. Biosimilars alone are projected to have global savings of up to $150 billion by 2027.7 So, why is there still a holdup to their wider implementation?
- Claims Cost Transparency: Using Data to Optimize Medical Benefits Costs. Employee benefits are the second largest budget item in employee compensation, with medical benefits consuming the bulk of that cost. Yet, companies with fully insured medical plans often have limited financial transparency and control when it comes to managing these costs. Try viewing the actual, full cost for a broken ankle, and you’ll see that pricing is not so transparent. Companies that know and understand their medical & Rx claims can make decisions that will improve plan utilization and reduce overall costs. Claims cost analysis allows you to drill down into the data and see what you need in your health plan to boost utilization and get your employees and their families better care. Many small and mid-size companies have fully insured plans, allowing for a fixed monthly cost. The carrier creates a pool, lumping your company with others. The carrier may determine your rate based on costs for the entire pool, meaning you’ll pay a set cost whether your company’s claims are higher or lower than average. When it comes to data, however, fully insured plans may not provide transparency or flexibility. They offer some claims data, but the carrier owns all of it, including your high claimant utilization.