This blog is for anyone wanting to reduce overutilization, waste, abuse, and fraud in a self-funded pharmacy benefit program.
- Define what it means to have a quality pharmacy benefits program then execute. Care structure should place a premium on making sure the drug works, making sure the drug is going to the right patient, and finally making sure the patient is taking the drug, for instance.
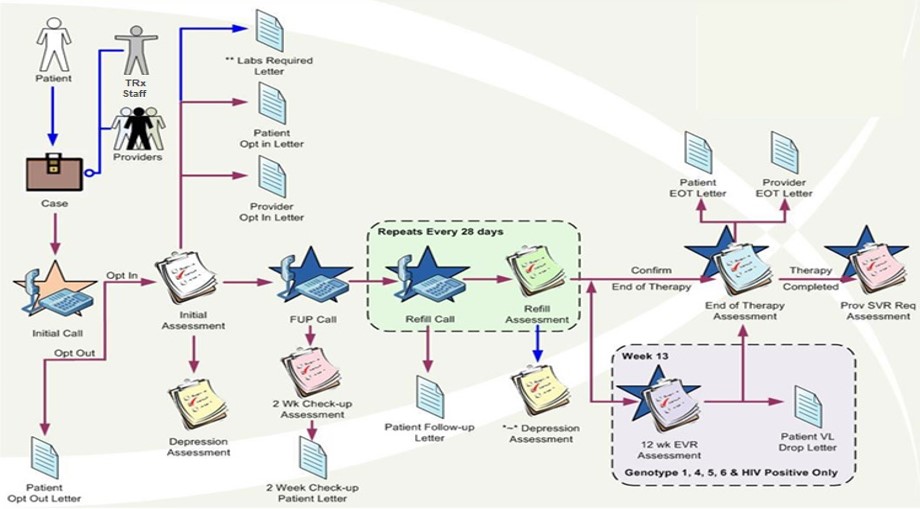
- Document and orchestrate processes. Specialty pharmacies must have disease state specific patient intake workflows. Take the emotion out of prior authorizations (and other utilization management programs i.e. step therapy) to deliver better results for patients and plan sponsors. The largest ePA or electronic prior authorization provider in the country is owned by a drug wholesaler. Systematize processes and don’t deviate.
- Reduce barriers to access. This doesn’t mean making every drug in the market available to anyone who has a prescription. It does mean that a patient prescribed the right drug should not be hindered by the plan design in taking said drug. A copay accumulator program is a strategy used by insurance companies and pharmacy benefit managers to stop manufacturer copay assistance programs from counting towards the deductible and out-of-pocket spending. These programs should be eliminated as they restrict access to drug therapies.
- Be relentless in pursuit of efficiency. Plan objectives should be accomplished with the least expensive combination of resources. Easier said than done and it all starts with PBM literacy.
- Quantify participant satisfaction. Net Promoter Score, or NPS®, measures customer experience, for example. A word to the wise, don’t sacrifice efficiency just to make a patient or doctor happy. Strive for above average participant satisfaction but stick to the documented plan. You can’t make everyone happy.
Conclusion
Reducing waste and abuse in pharmacy benefits starts with the five methods listed above. If the primary goal of drug therapy isn’t to achieve better health care outcomes, with the least expensive combination of resources, then what are we doing? Pharmacy benefits management isn’t a beauty contest.