In the evolving landscape of healthcare benefits, corporations find themselves at a crossroads, especially when it comes to covering weight loss medications like Wegovy. A recent development has seen Novo Nordisk, the pharmaceutical giant behind Wegovy, imposing penalties on employers who limit access to these expensive drugs, have led at least two major employers to discontinue their coverage, unveiling a weight loss drug coverage dilemma:
- Increased Healthcare Costs: Employers face rising expenses in providing health benefits, driven by the excessive cost of weight loss medications.
- Access and Affordability for Employees: Restricting or discontinuing coverage affects employees’ access to potentially life-changing treatments, raising questions about healthcare equity.
- Negotiation Dynamics: The power struggle between pharmaceutical companies, PBMs, and employers over drug pricing and discounts reveals the complex negotiations that underpin healthcare benefits.
- Corporate Responsibility and Employee Well-being: Companies must balance their financial constraints with their responsibility to support employees’ health and well-being.
- Broader Healthcare Debate: This situation contributes to the ongoing debate about drug pricing, insurance coverage, and the right to healthcare, highlighting the need for systemic changes in how medications are priced and covered.
The crux of the matter lies in the negotiation dynamics between employers, Pharmacy Benefit Managers (PBMs), and drug manufacturers. PBMs play a crucial role in negotiating drug prices, but their ability to secure discounts is being challenged by the manufacturer’s aggressive tactics. This situation leaves employers grappling with soaring healthcare costs, putting them in a difficult position: either absorb the excessive costs of these medications or face the manufacturer’s financial penalties.
The standoff has major implications for both companies and their health plans, as well as for employees dependent on these medications for their health. Despite a company’s financial resources, deciding whether to cover weight loss drugs remains a complex issue. Additionally, there’s a significant risk of fraud associated with GLP-1 weight loss medications. This concern arises from the potential for these drugs to be overprescribed, misused, or diverted, leading to unnecessary costs for companies without corresponding health benefits for users.
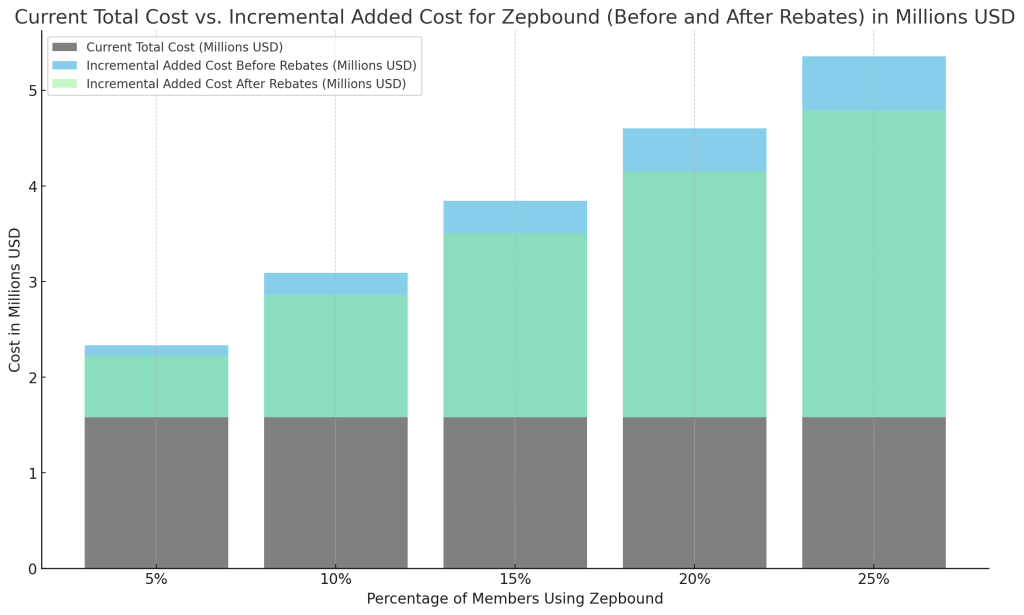
The bar chart (figure 1) could simplify this decision-making process regarding their inclusion in the formulary. I suggest holding off until prices decrease. Meanwhile, consider exploring other options such as diet and exercise. As corporations navigate this tricky terrain, the broader conversation about drug pricing, healthcare benefits, and corporate responsibility continues to evolve. This scenario underscores the complex interplay of financial, ethical, and healthcare considerations that companies must balance in the modern corporate landscape.