“If we just lowered the cost of Sovaldi from $85,000 to $50,000, every payer would rip up our contract,” said Jim Meyers, executive vice president of worldwide commercial operations, in an interview with Bloomberg News.
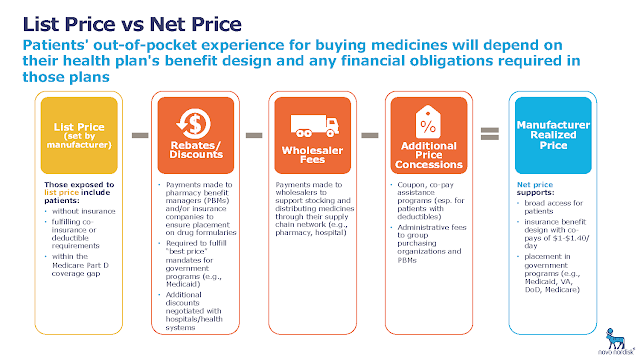 |
| Source: Novo Nordisk |
Pharmacy benefit managers such as Express Scripts Holding Co. and CVS Health Corp. negotiate drug reimbursement, often in secrecy, for employers and health plans. While PBMs say they deliver lower prices for customers and patients, drugmakers have begun aggressively implicating the middlemen in high medication costs that have become a frequent target of Washington lawmakers and President Donald Trump.
One of the functions of PBMs is to help insurers decide which drugs to cover for their customers, and how much to reimburse manufacturers. Manufacturers use rebates to ensure they get on PBMs’ lists of covered drugs, called formularies, and the middlemen often take a cut of those rebates, often about 10 percent, for themselves before passing the rest of the savings to the insurers. Now, pharmaceutical companies are charging that PBMs prefer higher list prices, because the middlemen want to sustain their own revenues.
“I have never met, in this entire experience, a PBM or a payer outside of the Medicaid segment that preferred a price of $50,000 over $75,000 and a rebate back to them,” Meyers said in the interview.