 |
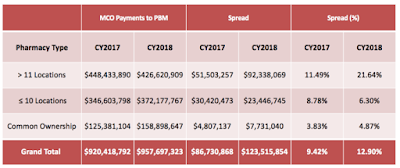
| Spread by Pharmacy Type |
Last year, pharmacy benefit managers, or PBMs, took in $123 million through a practice known as “spread pricing,” the difference between what the pharmacy benefit company pays the pharmacist and what it bills the state Medicaid program, according to the report.
Tyrone’s Commentary:
This should sever as a warning to all self-insured employers. Despite Kentucky’s best efforts to reduce PBM service fees, payments to PBMs grew year-over-year. Even as lawmakers increased scrutiny and passed legislation demanding more transparency, non-fiduciary PBMs still increased the amount of revenue they took in! If a state with unlimited resources can’t stem PBM service fees, how does a commercial employer even stand a chance? Here’s the answer. Do business with a fiduciary-model PBM. While the answer may seem self-serving it isn’t. There are just too many loopholes, from which a non-fiduciary PBM can benefit, for even the sharpest consultant, HR Executive or CFO to close. Leave just one loophole open and you will bleed out.
Kentucky’s Eight (8) Recommendations:
1) Mandate pass-through contracting for all MCO-PBM contracts for pharmacy.
2) Remove all DIR fees including transactional fees, in-network fees, GER and BER fees.
3) Evaluate the implementation of a pricing methodology to managed care Medicaid pharmacy. Using a similar lesser of logic methodology, medications would be reimbursed the same as Kentucky’s fee-for-service population.
[Read Full Report]