DUM or drug utilization management in specialty pharmacy helps to maximize efficiency. That employers don’t engage in wasteful spending and the right drug, at the right time gets in the hands of the right person. It likewise encourages digital monitoring of the member’s drug therapy in the past, the now and in the future. Here are three imperatives around specialty drug therapy to consider while designing a pharmacy benefit plan:
Specialty pharmacies use medication therapy management (MTM) to coordinate comprehensive care for patients and improve health outcomes. MTM employs a range of clinical tools to improve outcomes and promote value, including therapeutically focused clinical assessments, validated quality of life measures, detailed medication reconciliation, monitoring adverse effects, connecting patients to educational resources, peer-based support programs, and access to need-based financial resources reducing barriers to care. Specialty pharmacies provide patient level support reducing health system and therapy complexity by explaining benefits and coverage, coordinating the best site of care for injected or infused medication, providing drug administration training, adherence support, and resources empowering patients to independently manage complex, persistent treatment plans.
Imperative 2: Evaluate Parity in Pricing for Specialty Drugs
When a specialty medication is parity priced, the drug is the same price regardless of the dose prescribed. For instance, Pomalyst is manufactured in 1 mg, 2 mg, 3 mg, and 4 mg strengths. It is the same price for 1 mg as it is for a 4 mg dose. It is prescribed once per day. QD (qd or q.d.) is once a day; q.d. stands for “quaque die” (which means, in Latin, once a day). BID (or bid or b.i.d) is two times a day ; b.i.d. stands for “bis in die” (in Latin, twice a day). There is no therapeutic benefit for someone to take four 1 mg tablets as opposed to one 4 mg tablet, and yet this is something we see when repricing pharmacy claims files today. Imbruvica and Afinitor are other examples where these cases do not involve changing the drug nor changing the dose. Changing parity priced dosing can save $400K-$500K on a single prescription for a single patient.
 |
| Click to Learn More |
Imperative 3: Take a proactive approach to prior authorizations.
I’ve been fortunate enough to be a “fly on the wall” listening to the leadership teams of several national specialty pharmacies. And while they preach case management and patient care as the priority if you listen carefully what they really want first and foremost is volume or more prescriptions. I am asking self-funded employers a simple yet very important question. Does it make sense to have the same entity manage and approve specialty Rx claims when that entity stands to benefit when these claims are approved? If 85% or more of PAs are getting approved you might be a victim of rubber-stamping which leads to what? You guessed it – wateful spending. Just because you have a PA or step therapy program doesn’t mean it is efficient. Consider carving out the prior authorization process or use prior authorizations with a dollar limit. The goal is not to create disruption but to review the clinical appropriateness of any dose increases, for example.
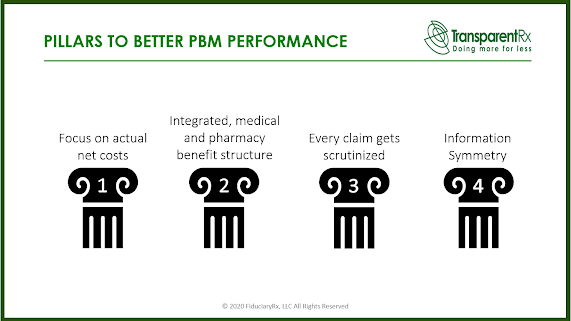
In conclusion, PBMs will generally manage costs to a level demanded by clients when negotiating their contracts. The best proponent of radical transparency or lowest net Rx cost is informed and sophisticated purchasers of PBM services. In other words, the more you know the less you pay without any reduction in member experience or outcomes.