In 2013, Ms. Potter noted, 17% of employers offered high-deductible health plans as their employees’ only option—up 31% from 2012, according to PricewaterhouseCoopers’ “Behind the Numbers 2014.” For 2014, she said, some 44% of employers were considering such a move (http://pwc.to/1eRYLxr).
High-deductible plans can pose challenges for anyone with a chronic condition, but they are particularly problematic for patients taking expensive specialty medications, with annual minimum deductibles of $1,250 per person and $2,500 per family. The 2014 annual cap on out-of-pocket costs is $6,350 for an individual and $12,700 for a family—high for anyone, but harder to swallow if it’s front-loaded into the first month or two of each year because of costly specialty drugs.
Those steep costs can be a powerful trigger for noncompliance. In one study, high-deductible health plans were found to reduce adherence to prescription medication regimens in four of five conditions evaluated: hypertension, dyslipidemia, diabetes and depression (Am J Managed Care 2013;19:e400-e407), Ms. Potter noted. Only in asthma/chronic obstructive pulmonary disease was there not a significant decline in adherence.
The conditions included in the compliance study generally do not require specialty medications, Ms. Potter pointed out; it’s thus possible that the documented adherence problems might be even more pronounced when it comes to specialty medications, “particularly because few of these drugs have generic alternatives in a lower tier, and patients may have to pay $7,600 or more per year out of pocket for specialty medications,” she said.
Health Exchanges Not Immune
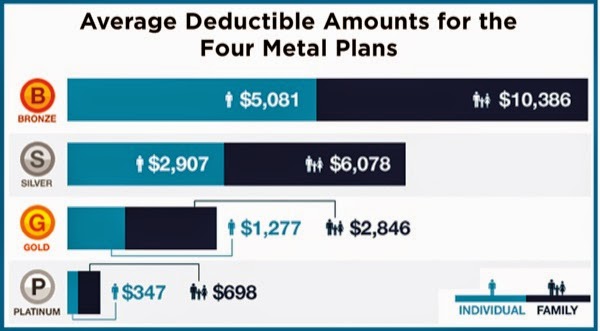
If employer-sponsored plans are increasingly moving toward high deductibles, many plans on the new health insurance exchanges—especially at the lower bronze “metal level”—are already there. In December, HealthPocket Inc., which compares health insurance plans for consumers, found that the average annual individual deductible for a bronze plan was just over $5,000, in addition to the average premium of $295.51 a month, or $3,546 a year (http://bit.ly/1oevFqq).
“These high-deductible plans are causing a bit of a problem,” Debbie Stern, president of Rxperts, told Specialty Pharmacy Continuum. “It’s really putting a high burden on the patient to come up with all of that up front. Even if it’s just a $2,000 deductible, the patient has to pay that up front almost immediately for most specialty drugs, so the first prescription is going to cost them almost the full out-of-pocket for the year. When these plans were designed, people were thinking of drugs that cost $200 a month, not specialty drugs that cost $2,000 a month or more.”
Here’s where good specialty pharmacies can really distinguish themselves, Ms. Potter said. “You can provide additional patient support, working proactively to help patients understand their medical plans and anticipate their financial demands.” (See sidebar for more details on these strategies.)
That’s already happening at many specialty pharmacies around the country, according to Kyle Skiermont, PharmD, the director of specialty/infusion operations at Fairview Pharmacy Services in Minneapolis. “We’re seeing a big increase in high-deductible plans, along with a rise of coinsurance,” Dr. Skiermont said. “We’re seeing both more patients with these plans, as well as higher dollar amounts they’re needing.”
Fairview has doubled its staff of patient financial advocates over the past year to help address the growing need. And it’s not just that more patients need assistance—their situations are also becoming more and more complicated, Dr. Skiermont noted. “Where one advocate might have been able to handle many more patients in the past,” he said, “each patient we are helping is taking more time and getting more complex in [his or her] needs.”
Many of the foundations and other sources of funding for medication assistance are also getting tapped out more quickly. That, too, requires creativity. “Some foundations recharge their funds over the year, so if you ask for a grant on behalf of your patient and it’s not there, you need to know when to go back to them,” Dr. Skiermont said. “Maybe there was no funding in March but there may be in October. It requires a lot more interaction and advocacy for our patients, multiple times a year, whereas historically we might have only needed to do that once a year.”
“We’ve been getting more and more creative around what we can do as far as payment plans,” Dr. Skiermont added. “If we know someone has a big out-of-pocket maximum that they’re going to hit in the first month, we’ll try to make arrangements to pay that over the year.”
It’s a patchwork solution that likely is not sustainable in the long term. “In the short term, we feel we owe this to our patients. As a nonprofit, health-system–based specialty pharmacy, providing this kind of high-touch financial assistance is one of our differentiators.
It’s core to our mission,” Dr. Skiermont said. “We need to continue to be innovative and make this work for our patients, but ultimately something is going to have to change. A lot of the burden is falling on specialty pharmacy, but at the same time, the providers and the pharmaceutical companies are beginning to understand the coverage issues better than they did a couple of years ago, and are helping us bring the message to the patient. The reality is that everyone’s still trying to figure this out.”
by Gina Shaw