 |
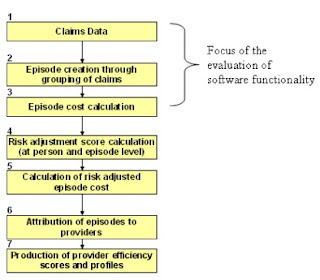
| Figure 1. Stylized Procedure for Using Episode Groupers to Evaluate Provider Efficiency |
Executives should care because specialty drugs used to treat many common chronic conditions are covered under both benefits; managing in the silos sub-optimizes clinical and cost management,” said John Fox, MD, senior medical director at Priority Health, who spoke at an online workshop from the Academy of Managed Care Pharmacy and The Pharmacy Group.
“Further, integration of utilization data, benefits, and management allows application of common principles across all benefit designs regardless of whether or not the drug is covered under the medical benefit, the pharmacy benefit or a separate specialty drug rider,” Fox said.
Top Integration Advantages
• Creation of a single P&T committee
• Guiding principles can be applied across benefits
• Management of disease states rather than benefits
• Application of cost-containment levers regardless of benefit
• Step therapy across benefits
• Presentation of a common formulary to consumers and providers regardless of benefit
• Optimization of rebates
• Reduction in adverse selection by adoption of comparable tiering and cost sharing structures on both the medical and pharmacy benefit
Michigan-based Priority Health, a nonprofit health plan offering a broad portfolio of health benefit options for employer groups and individuals, including Medicare and Medicaid plans, recently saw that more than half of the premium price increase was due to drug trend.
Almost 40% of the drug spend is on specialty drugs yet only 0.9% of patients utilize specialty drugs, said Fox. As such, it is imperative that it uses any reasonable tool to ensure that the drug spend is clinically and financially appropriate.
At Priority Health, the top four chronic conditions in specialty drug spend for commercial and Medicaid products are:
1. Multiple sclerosis
2. Psoriasis
3. Rheumatoid arthritis
4. Inflammatory bowel disease (IBD).
For multiple sclerosis, 8% of spend is on drugs covered under the medical benefit and for IBD, 38%.
In Medicare, the top spends are multiple sclerosis, leukemia, multiple myeloma and macular degeneration. For multiple myeloma, 16% of the spend is on Part B drugs and for macular degeneration, 100%.
“These data highlight the importance of having an integrated strategy for managing across medical and pharmacy benefits,” Fox said. “For example, in IBD, the plan requires failure of the pharmacy-benefit drugs before use of alternative drugs covered on the medical benefit.”
Prior to implementing this tactic, the spend for medical benefit drugs was more than 50% and cost PMPM significantly higher, according to Fox. “For macular degeneration, all drugs are managed through a prior authorization process that monitors dose, frequency and response to therapy and requires use of preferred agents in a step therapy process,” he said.
“For cancers and hematologic malignancies, there is no preference for a medical benefit drug or a pharmacy benefit drug, but selection is influenced by cost sharing on the preferred and non-preferred specialty tiers on both the medical and pharmacy benefit. Providers and patients alike can access the integrated web-based formulary and any limitations across both benefits.”
Priority Health integrates data from the medical and pharmacy benefits through the Symmetry Episode Treatment Grouper (ETG). The grouper assigns all claims, both medical and pharmacy, into disease-specific ETGs (see figure 1).
The ETGs are then searched for any specialty drug. A list of drugs included in each ETG is then compiled and represented graphically or tabularly. Total spend and trend changes are monitored on a monthly basis by the drug trend management group.
By Tracey Walker