The Mississippi Division of Medicaid confirmed the probe to the Daily Journal on Monday. Medicaid officials said the attorney general’s office hired outside attorneys to “investigate and potentially pursue claims” that include Centene’s management of pharmacy benefits.
Tyrone’s Commentary:
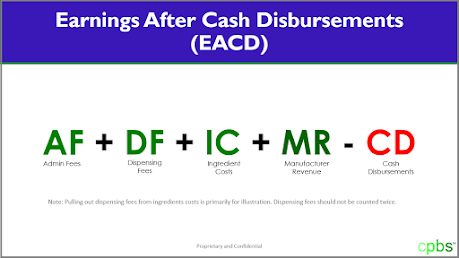
States have pivoted from evaluating PBM performance on discount guarantees and rebates to the PBM’s management fee. EACD or the PBM management fee is the amount of money a PBM is being paid to provide its services. It is only after you know how much money a PBM is taking home that you begin to realize the magnitude of overpayments. Running an efficient pharmacy benefits program requires sophistication, bravery and steadfastness.
 |
| Click to Learn More |
In my business, I’ve always recommended a continuous monitoring process. Continuous Monitoring or CM would have identified Ohio’s and Mississippi’s problems before they got out of hand. This of course assumes you have the right advisor working on your behalf. Most don’t know the difference between a ZBD claim and a clawback. But I digress. Audits occur 12 – 24 months after the fact which is too late to recoup the majority of overpayments. Continuous Monitoring on the other hand, catches and resolves overpayments or other issues much faster. Even with the full power of the AGs office, I’d be surprised if the plaintiffs win.
The investigation is in the early stages but is similar to a recently-announced Ohio lawsuit against Centene, said Colby Jordan, a spokeswoman for Attorney General Lynn Fitch. In that case, authorities allege Centene overcharged Ohio taxpayers by millions of dollars.
The Ohio suit, according to Yost, alleges three areas of wrongdoing: requesting reimbursements for amounts already paid by the state, failing to disclose the true cost of pharmacy services, and artificially inflating drug dispensing fees. Yost’s office suggested that Centene’s practice of subcontracting with more than one firm to provide pharmacy benefits had raised red flags.
In Mississippi, Magnolia Health uses at least two companies – Envolve Pharmacy Solutions and RxAdvance – to get drugs to Medicaid recipients, according to a 2019 Centene news release.