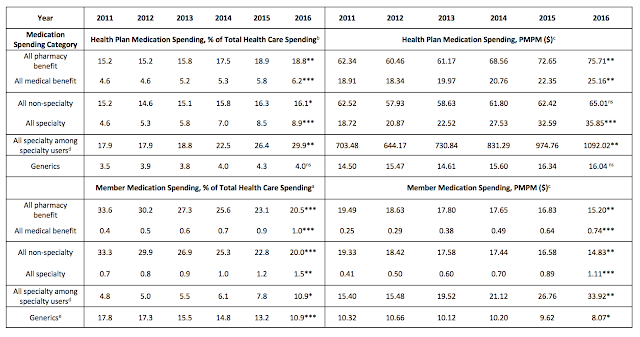
At 25 percent of total health care expenditures in 2016, net spending on pharmaceuticals by Harvard Pilgrim Health Care (HPHC) was consistent with retail pharmaceutical spending proportions of commercial payers across states and considerably higher than 10 percent to 17 percent often reported nationally.
 |
| Click to Enlarge |
At HPHC, considering only pharmacy benefit spending would fail to account for the 25 percent of medication spending attributable to those medications administered in physicians’ offices and paid under the health plans’ medical benefit—similar to an estimated national 28 percent spending contribution of non-retail medications.
Tyrone’s Commentary:
1 in 4 dollars attributed to prescription medications and this doesn’t include spend on inpatient HCPCS J Code drugs! Soon the DOJ will approve the mergers of CVS/Aetna and ESI/Cigna. Like Optum and Prime Therapeutics, CVS and ESI want to capitalize on the potential of inpatient medical spend J code drugs. The PBMs will bring with them all of their knowledge and drug utilization management tools which is a great opportunity to improve patient outcomes and contain costs. Unfortunately, it also gives them the chance to add to costs. Because PBMs generally rely on the demands of clients for the level of transparency provided, the scenario which plays out is largely up to plan sponsors and their advisers. When you know better, you do better.
It is noteworthy that our pharmaceutical spending estimates exclude payments for inpatient-administered medications, as those are included in inpatient spending. Consequently, our data understate total pharmaceutical spending.