Midwest Business Group on Health or MBGH has drawn a line in the sand. In order to help employers
improve the efficiency and value of pharmacy benefit programs to drive affordability and transparency, the Midwest Business Group on Health recently released a new report.
 |
| Click to Learn More |
Tyrone’s Commentary:
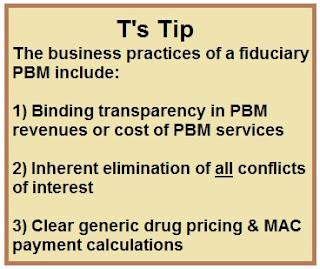
Seems that MBGH and TransparentRx have a lot in common at least in choice of words. Actions are what matter most.
The report offers a call to action on the key issues and important steps that public and private employers need to take to:
- Understand how “today’s middleman model” contributes to higher costs in the supply chain
- Identify ways to work with vendors to reduce unnecessary costs and drive efficiency
“As fiduciaries, employers have a duty to be ‘good stewards’ of how premiums are used to fund care for employees and beneficiaries,” said Cheryl Larson, MBGH vice president and primary report author, when announcing the report. MBGH non-profit employer coalitions of 130 mid, large and jumbo self-funded public and private employers, representing over 4 million lives and annually spending over $4 billion on health care.
“Most pharmacy benefit manager (PBM) arrangements are complex, making it difficult for employers to identify the true cost of drugs and all the sources of PBM revenue,” Larson added. “Employers need to know the facts and act to make sure their benefit dollars are spent in an efficient manner and rebates and other revenues are appropriately received.