ICER’s New Final Report on Anti-Obesity Drugs: The Days of Blanket Exclusions Are Numbered
Obesity drugs are back in the spotlight, and not because people suddenly discovered willpower. It’s because the newer GLP-1 and dual GLP-1/GIP medications have changed what’s medically possible for weight loss. Semaglutide (Wegovy) and tirzepatide (Zepbound) are producing results closer to bariatric surgery outcomes than anything most employers have seen from traditional weight management programs. For self-funded employers, the real question isn’t “Do these drugs work?” It’s “What happens to our plan when demand explodes?”
That’s where ICER’s new final report on semaglutide and tirzepatide for obesity matters. ICER, the Institute for Clinical and Economic Review, is an independent nonprofit that evaluates treatments using a public, evidence-based process that weighs clinical outcomes and cost side-by-side. In this review, ICER evaluated injectable semaglutide 2.4 mg, oral semaglutide 25 mg (still under review for obesity), and tirzepatide 15 mg for adults with obesity who do not have diabetes. They also bring the evidence to an independent advisory council (NE CEPAC) for public votes on comparative benefit and value.
On the clinical side, ICER’s takeaway was clear: these drugs deliver meaningful outcomes when added to lifestyle intervention. In the trial evidence ICER summarized, tirzepatide produced an average 17.8% greater weight loss than placebo, injectable semaglutide produced 13.1% greater weight loss than placebo, and oral semaglutide produced 11.4% greater weight loss than placebo. Tirzepatide also outperformed semaglutide in a head-to-head trial, with a 20.2% reduction in body weight vs. 13.7% for semaglutide at week 72. Weight loss is what gets the headlines, but employers care about what this changes downstream.
ICER highlighted cardiovascular outcomes that connect obesity treatment to fewer catastrophic claims. In the SELECT trial population (adults with obesity and established cardiovascular disease), injectable semaglutide reduced major adverse cardiovascular events by 20% and reduced all-cause mortality. Once a drug category starts showing fewer heart attacks and fewer deaths in the right population, it stops being viewed as a cosmetic category and starts looking like cardiometabolic care.
ICER’s evidence ratings reinforced that shift. They rated injectable semaglutide, oral semaglutide, and tirzepatide as having high certainty of substantial net health benefit when compared with lifestyle modification alone. NE CEPAC unanimously agreed the evidence is adequate to show all three therapies deliver greater net health benefit than lifestyle changes alone. At the same time, ICER and the panel didn’t give employers a simple “winner” between tirzepatide and semaglutide overall. Even though tirzepatide drives greater weight loss, the council overwhelmingly said the evidence is not adequate to distinguish a difference in net health benefit versus injectable semaglutide. That matters because employers are going to be pressured to chase the “stronger” drug, even when the long-term outcomes picture is still evolving.
Then the report turns to what employers feel immediately: cost. ICER’s modeling suggests these drugs can be cost-effective at commonly used thresholds. But they also estimated fewer than 1% of eligible patients could be treated at current and assumed net prices before crossing ICER’s national budget impact threshold, which is why they issued an access and affordability alert for semaglutide and tirzepatide in obesity.
Here’s the report’s message in practical terms for self-funded employers:
- ICER’s clinical conclusion is strong: these therapies provide substantial net health benefit versus lifestyle intervention alone.
- The most important “outcomes” story isn’t the scale, it’s reduced cardiovascular risk in the right population.
- Tirzepatide leads on weight loss, but ICER did not treat it as a proven “better overall” option versus semaglutide.
- ICER’s affordability warning is the real business issue: budget impact becomes unmanageable quickly if adoption scales.
- Stopping therapy often leads to weight regain, so coverage behaves like a long-term decision, not a short-term perk.
This report also suggests obesity drug coverage is drifting from “optional” to “hard to avoid.” ICER doesn’t say every plan must cover these medications, but they lay out the ingredients that push employers in that direction. When a therapy earns a high-certainty clinical benefit rating, when it shows cardiovascular event reduction in a high-risk population, and when demand is already growing, blanket exclusions become harder to defend.
Even employers who exclude weight loss drugs still end up dealing with the pressure through appeals, exceptions, provider complaints, and employee dissatisfaction. And once members start therapy, unstable coverage creates its own problem. ICER notes that stopping treatment often leads to weight regain and reversal of metabolic improvements. That means inconsistent coverage isn’t neutral. It creates a start-and-stop pattern that’s clinically messy and financially inefficient.
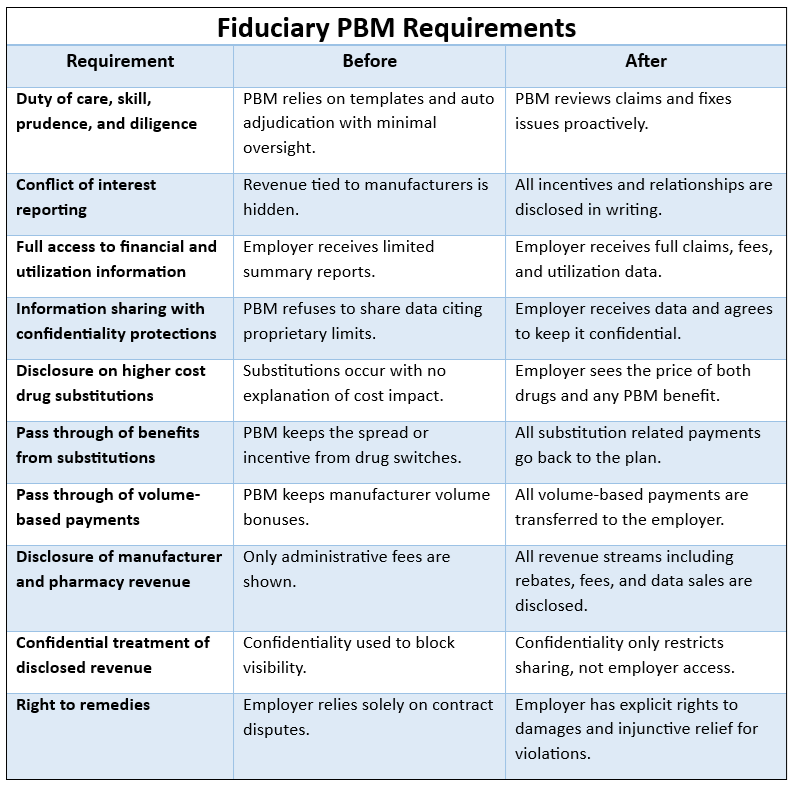
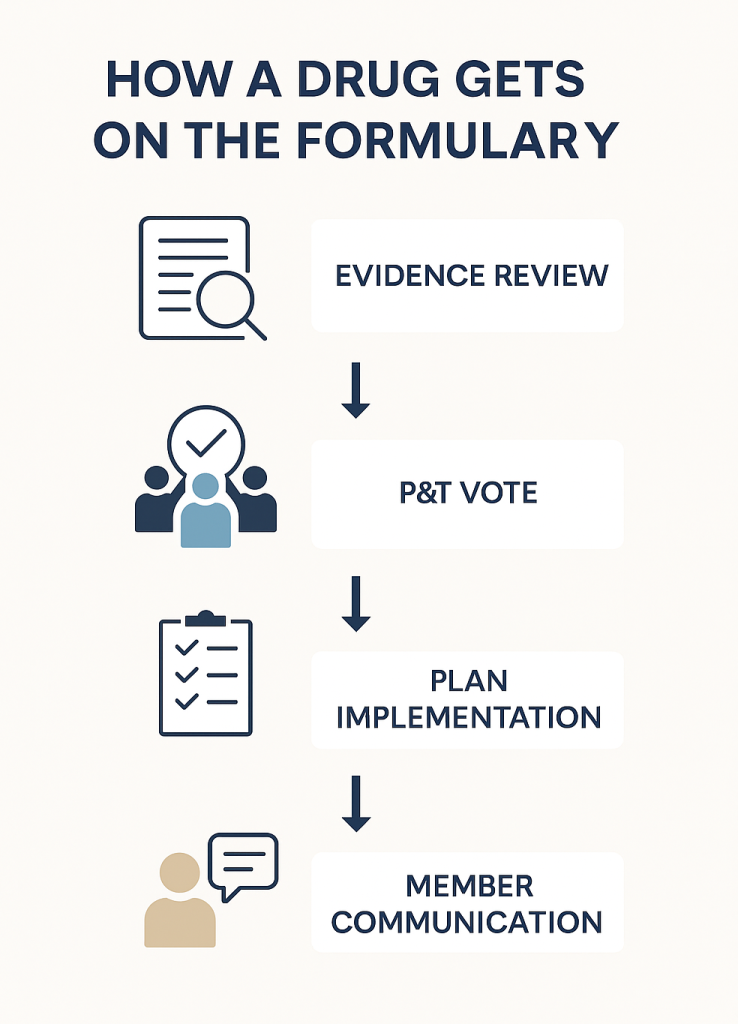
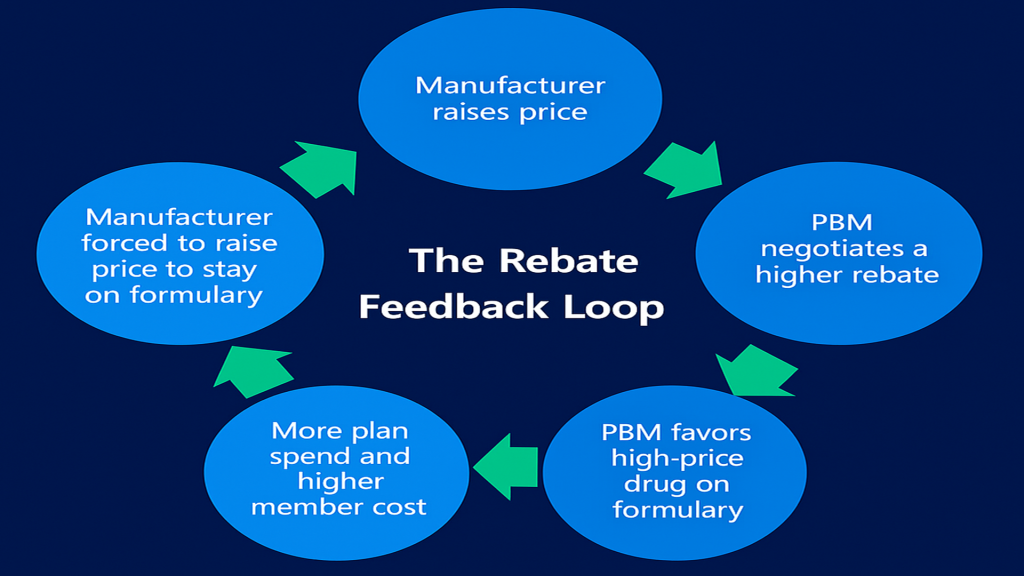
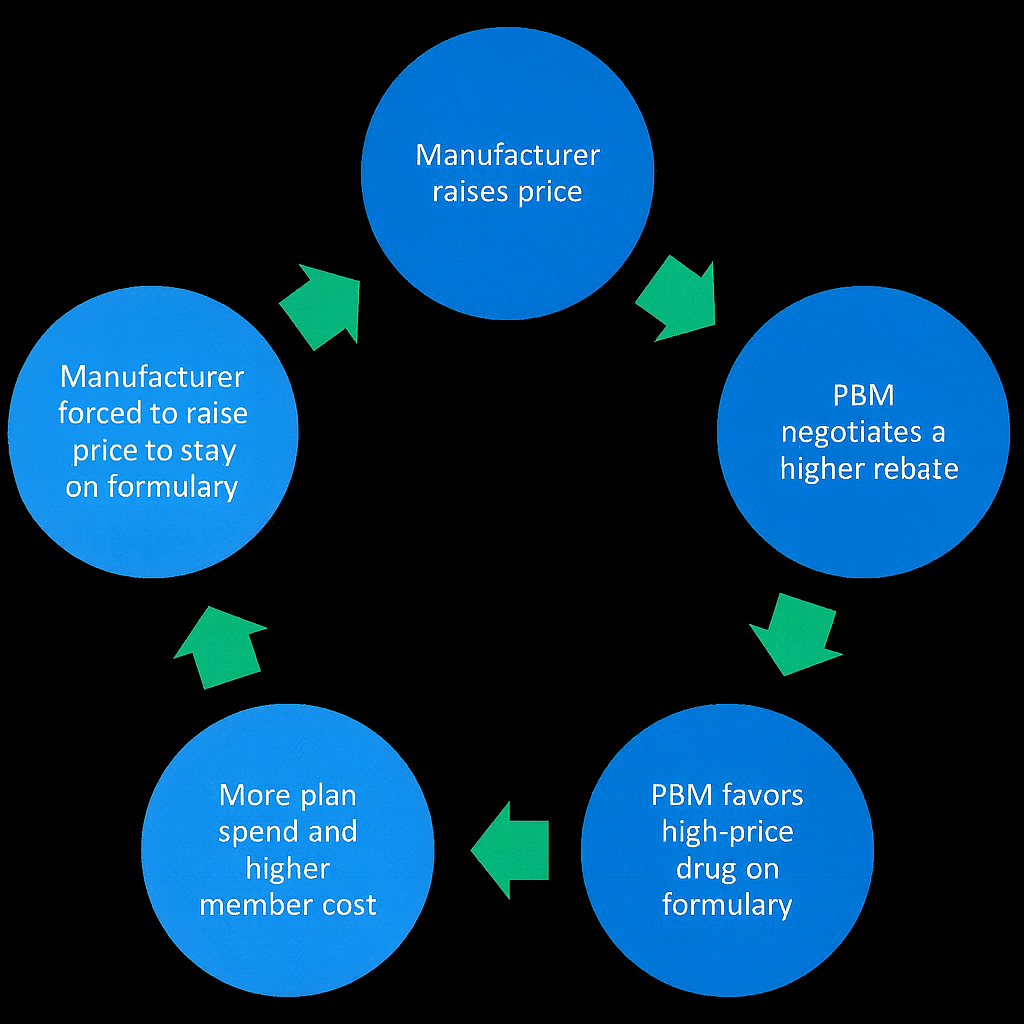
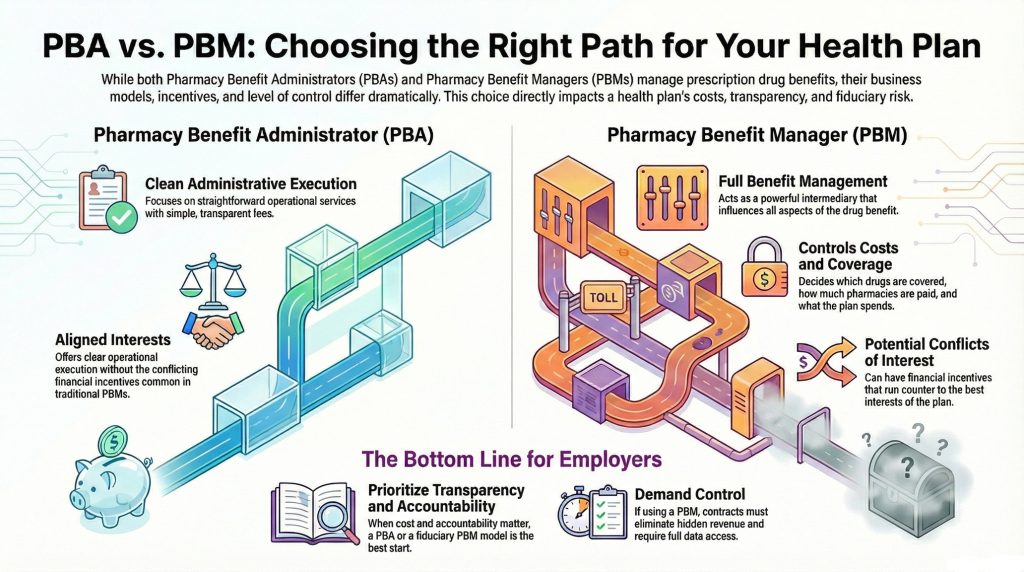
The practical employer takeaway is not “say yes” or “say no.” It’s that self-funded plans need to stop treating GLP-1 coverage like a simple pharmacy checkbox. Employers need a disciplined, defensible obesity strategy that reflects a fiduciary standard of care. That includes defined eligibility rules, consistent prior authorization, reauthorization tied to progress, outcomes tracking, and PBM accountability that’s built around total plan performance, not rebate math.
ICER’s report makes one thing clear: obesity treatment is no longer just about the scale. It’s about risk, long-term health outcomes, and whether employers can manage coverage with discipline before costs manage them instead.
How We Can Work Together
Whether you’re a plan sponsor trying to get control of pharmacy spend, or a broker guiding clients through PBM decisions, education is the fastest way to improve outcomes. If you want a focused, high-value session your team can actually use, here are three ways we can work together.
Option 1: Virtual Roundtable – Bring your internal team (HR, Finance, and Benefits) or your broker group. I’ll lead a live discussion focused on PBM oversight, cost drivers, and what to ask your PBM right now. You’ll leave with a short action list you can use immediately.
Option 2: Webinar – A clean, educational session for employers, brokers, or TPAs. We’ll cover the most common PBM profit tactics, how to spot contract red flags, and what a fiduciary standard of care looks like in pharmacy benefits. Great for client education and thought leadership.
Option 3: Quick Call – If you want a second set of eyes on your PBM contract, renewal, or pharmacy strategy, you can book a short meeting with me. No pitch, no pressure, just a practical conversation to help you figure out what to do next.
Book a Virtual Roundtable, Webinar, or Quick Call today. Choose your session type and reserve your date so your team can secure clear, fiduciary guidance on PBM oversight this week.