Tuesday Tip of the Week: 3 Common Places PBM Overcharges Occur
 |
| Click to Learn More |
 |
| Click to Learn More |
Always include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to determine if better pricing is available in the marketplace compared to what the client is currently receiving.
 |
| Aspirin (non-biologic) vs. Monoclonal Antibody (biologic) |
 |
| Click to Learn More |
Always include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to determine if better pricing is available in the marketplace compared to what the client is currently receiving.
 |
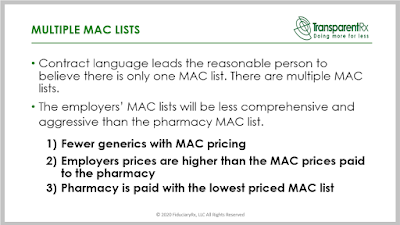
Click Here to View the Original Job Ad and Description |
Always include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to determine if better pricing is available in the marketplace compared to what the client is currently receiving.
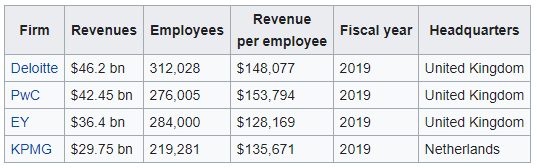 |
| Source: Wikipedia |
“Thank you! Awesome presentation.” Mallory Nelson, PharmD
“Thank you Tyrone for this informative meeting.” David Wachtel, VP
“…Great presentation! I had our two partners on the presentation as well. Very informative.” Nolan Waterfall, Agent/Benefits Specialist
A snapshot of what you will learn during this 30-minute webinar:
Sincerely,
TransparentRx
Tyrone D. Squires, MBA
10845 Griffith Peak Drive, Suite 200
Las Vegas, NV 89135
866-499-1940 Ext. 201