Astronomical prices of specialty drugs that treat hepatitis C, rheumatoid arthritis, cancer and other diseases are leading overall U.S. consumer prescription drug costs higher, according to pharmacists, pharmacy benefit managers and industry experts.
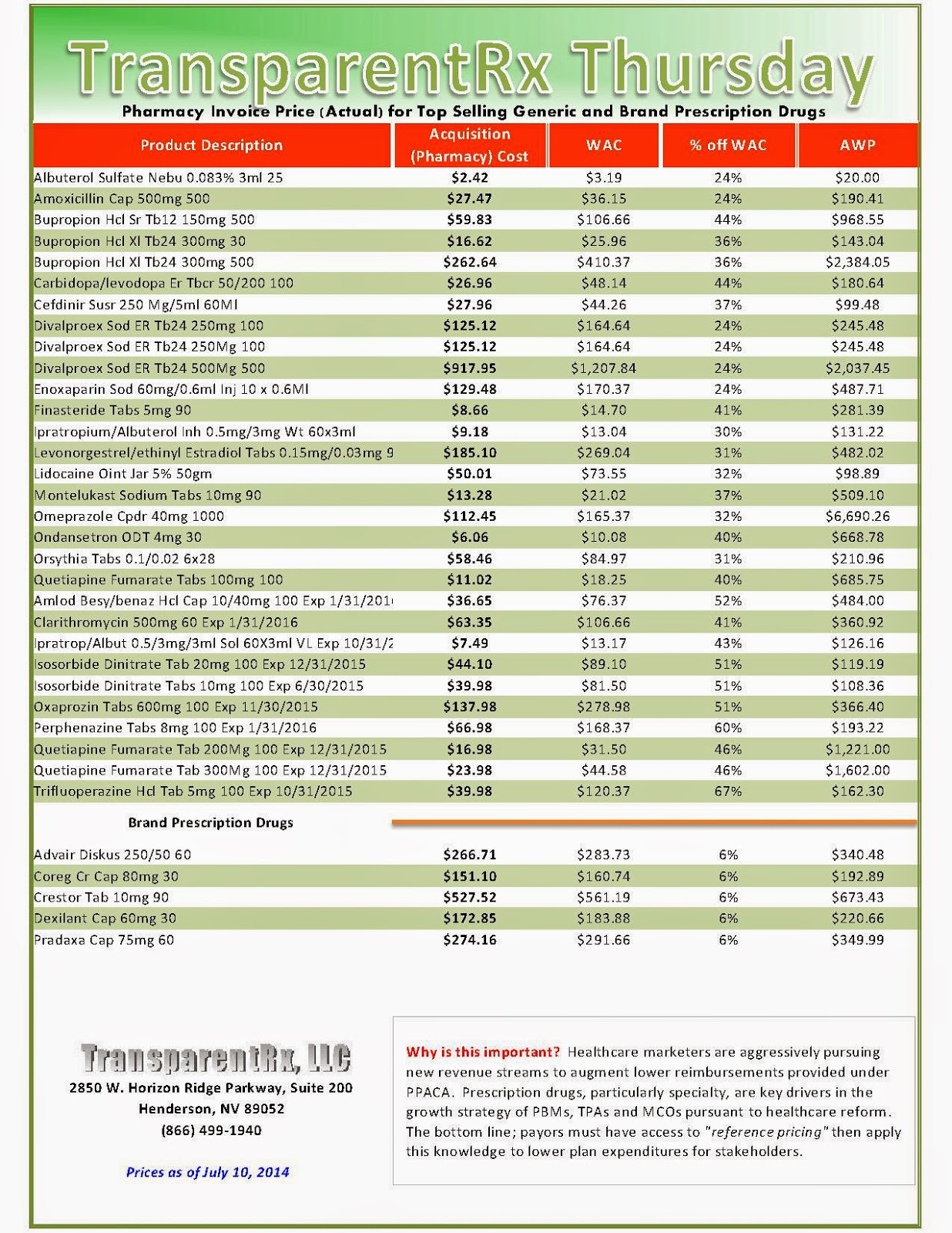
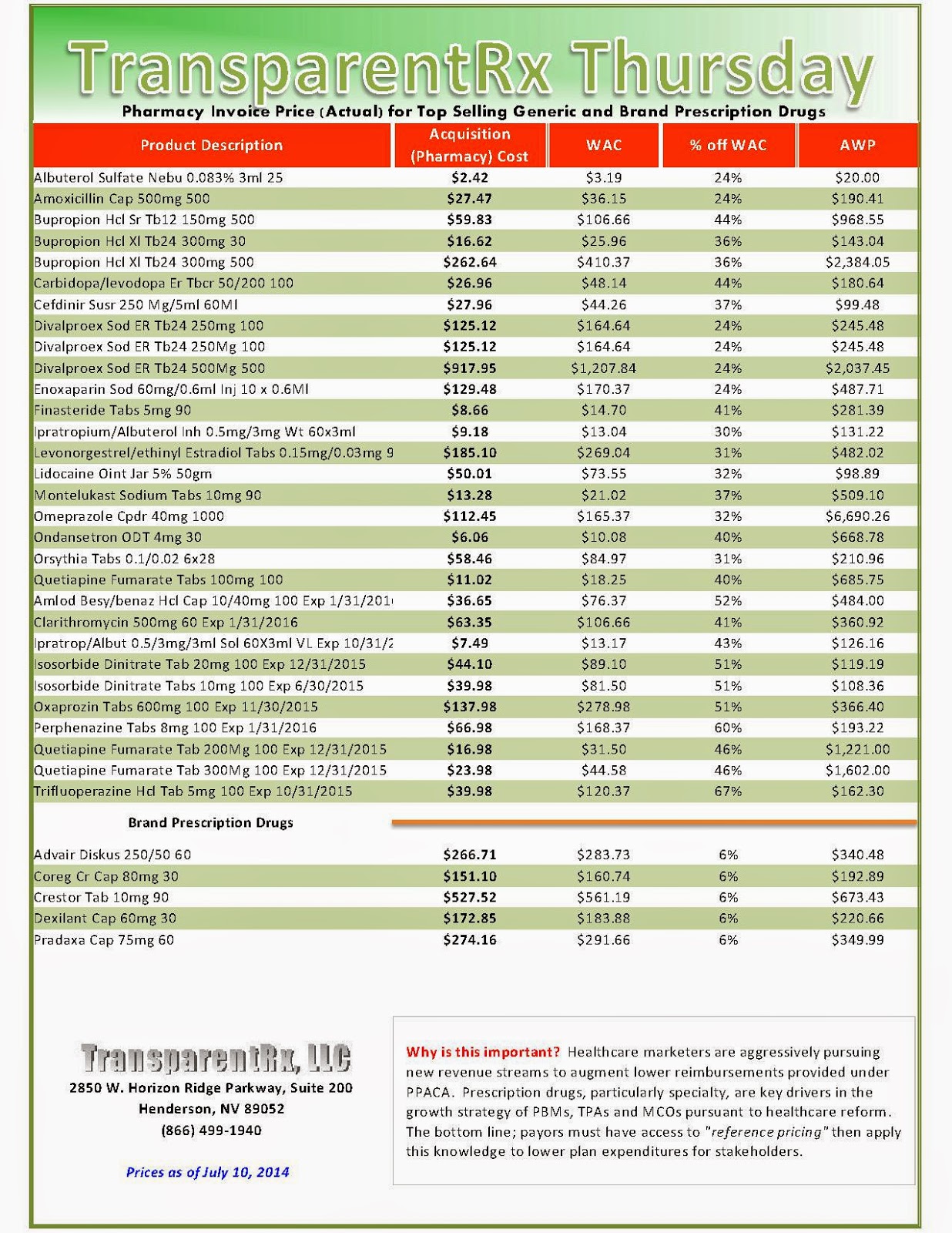
 Druggists and industry experts told MNI that traditional brand-name and generic drugs prices are also firming. Right alongside that, healthcare cost-sharing for prescription drugs continues to shift toward employees and others insured, by way of deductibles, co-payments, drug coverage exclusions and percentage coverage, also known as co-insurance.
Druggists and industry experts told MNI that traditional brand-name and generic drugs prices are also firming. Right alongside that, healthcare cost-sharing for prescription drugs continues to shift toward employees and others insured, by way of deductibles, co-payments, drug coverage exclusions and percentage coverage, also known as co-insurance.
The moderating impact on costs in recent years from a wave of blockbuster brand-name drugs going generic, from Lipitor to Lexapro, has faded, they said. A pharmacy benefit management company forecasted accelerating prescription-drug cost increases in 2014 for both consumers and insurers.
“It’s growing substantially this year because of the introduction of the new products in the hepatitis-C market. It’s very exciting but extremely dynamic in terms of its impact on cost this year on many of our plans,” said Peter Wickersham, senior vice president of integrated care and specialty at Prime Therapeutics, a PBM that helps control costs for 23 Blue Cross Blue Shield companies and other insurers that cover a combined 25 million members.
Total prescription drug costs, borne by consumers and Prime Therapeutics’ insurers, rose an average of 3.3% in 2013 from 2012, compared to 2.1% inflation the year before, in part due to increased utilization, Wickersham said.
“That’s about to change greatly,” Wickersham told MNI, and added that aggregate drug cost inflation should come in “north of 10%” this year, thanks in great part to Solvaldi, the hepatitis-C medication.
Specialty drugs cost insured consumers an average of $142 per prescription per month in 2013, up 15% from 2012, Wickersham said. The average specialty drug itself cost insurers $3,150 per month in 2013. Sovaldi comes in at a whopping $85,000 for a 12-week course, or about $1,000 per pill, he said.
Specialty drugs, Wickersham said, treat a relatively narrow population and comprise just 1% of total prescriptions filled. Yet by 2018, they could account for 50% of total drug costs, he said. And they aren’t the only medicine outlays on the rise.
“Starting toward the end of last year, we saw some price inflation on generic products, as well,” Wickersham said. While most generic prices are by and large stable, some “individual products are taking large price increases,” he said.
Read more here: https://mninews.marketnews.com/index.php/reality-check-us-consumer-drug-costs-climb-ever-higher?q=content/reality-check-us-consumer-drug-costs-climb-ever-higher
_1.jpg)

_1.jpg)


_1.jpg)

_1.jpg)
