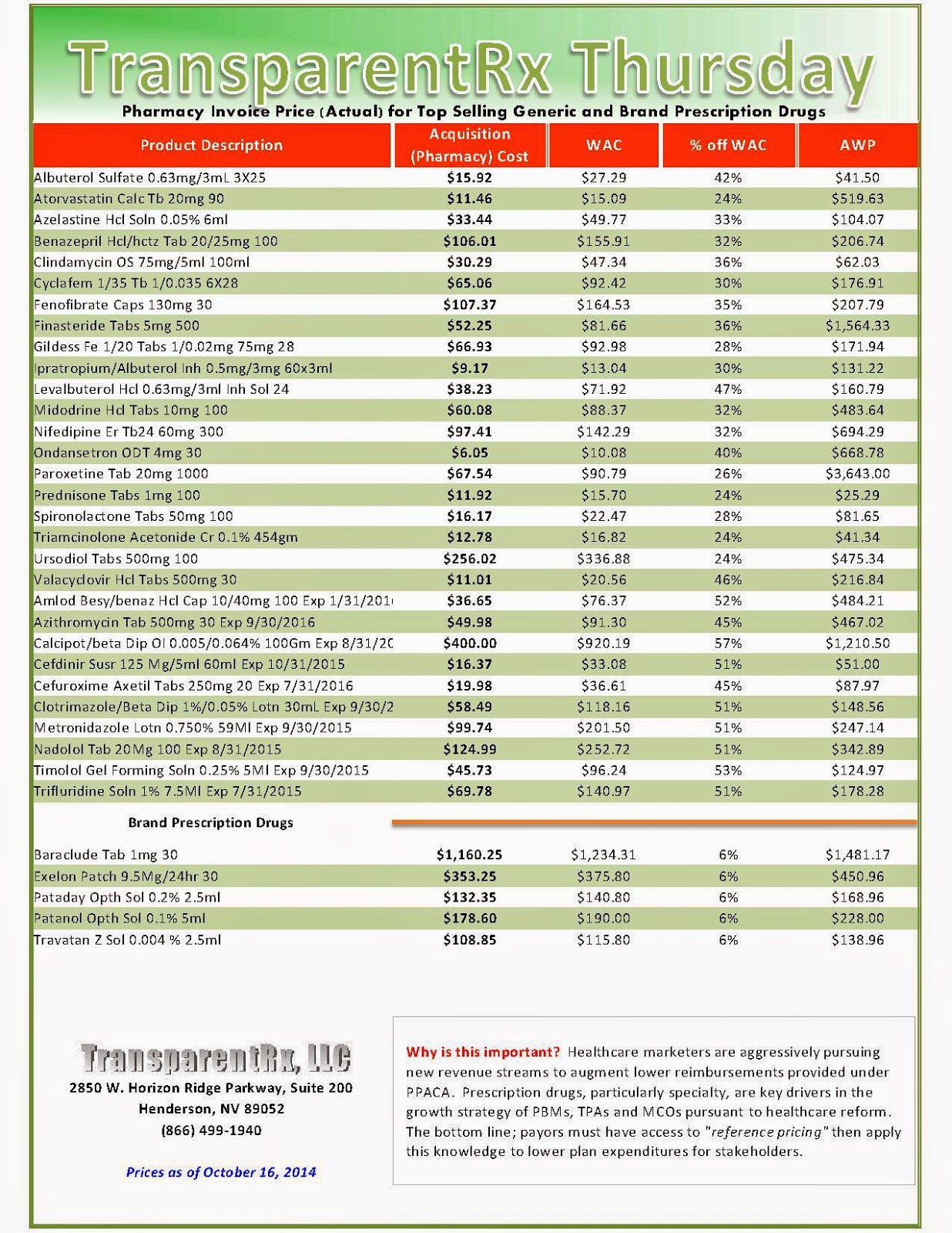
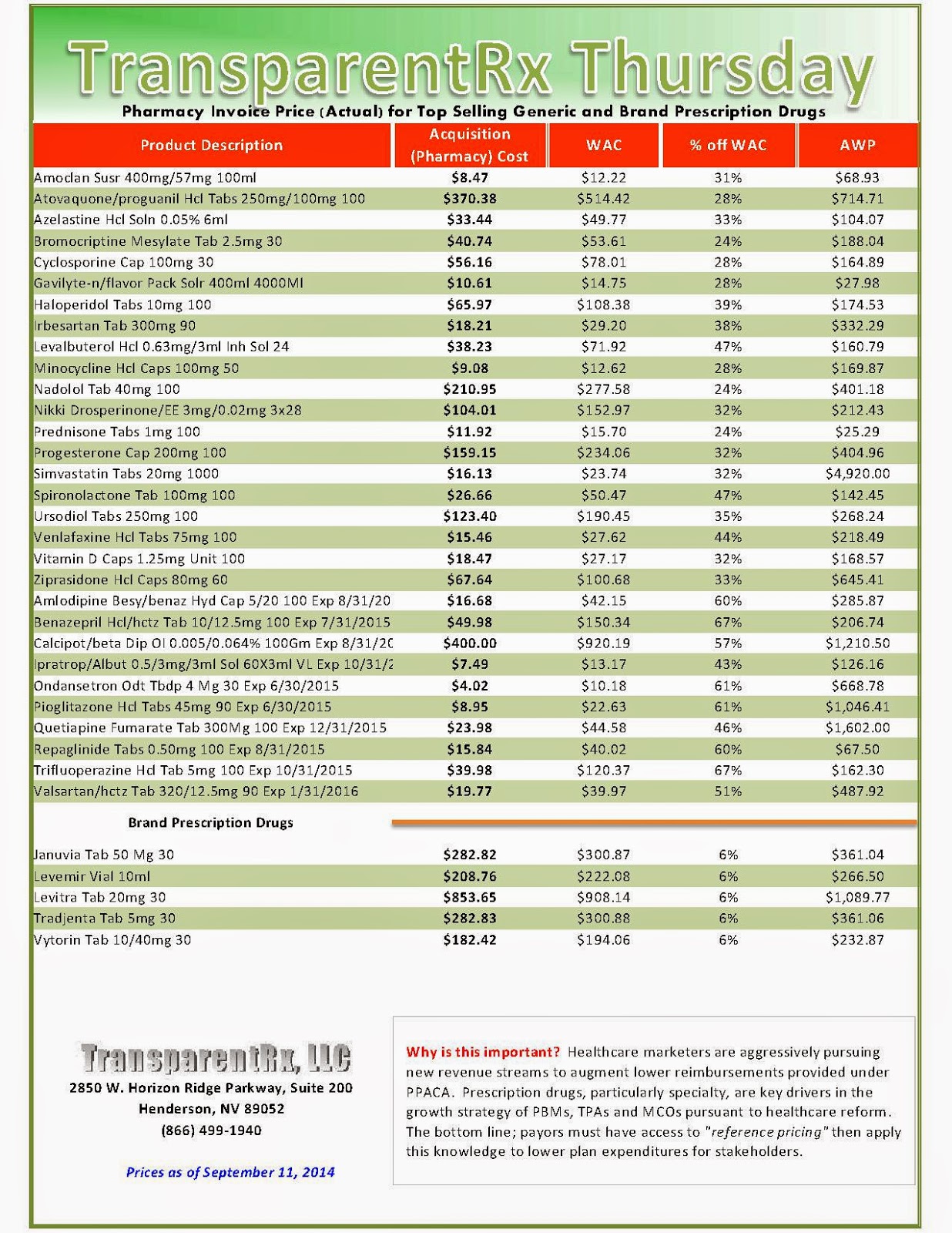
Reference Pricing: Pharmacy Invoice Cost (ACTUAL) for Top Selling Generic and Brand Prescription Drugs
The costs shared below are what our pharmacy actually pays; not AWP, MAC or WAC. The bottom line; payers must have access to “reference pricing.” Apply this knowledge to hold PBMs accountable and lower plan expenditures for stakeholders.
Note: This document is updated weekly to reflect changing prices and new products.
| How to Determine if Your Company [or Client] is Overpaying |
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our pharmacy cost then determine if a problem exists. When there is a 5% or more price differential (paid versus actual cost) we consider this a problem.
When better pricing is discovered the contract language should stipulate the client be indemnified. Do not allow the PBM to limit the market check language to a similar size client, benefit design and/or drug utilization. In this case, the market check language is effectually meaningless.
Click here to register: “How To Slash the Cost of Your PBM Service, up to 50%, Without Changing Providers or Employee Benefit Levels.” [Free Webinar]
National Health Expenditure Projections 2013-2023
- Health spending is projected to grow at an average rate of 5.7 percent for 2013-2023, 1.1percentage points faster than expected average annual growth in the Gross DomesticProduct (GDP).
- Health spending growth for 2013 is projected to have remained slow at 3.6 percent due tothe modest economic recovery, the impacts of sequestration and continued slow growth in the utilization of Medicare services, and continued increases in cost-sharing requirements for the privately insured.
- Improving economic conditions, the Affordable Care Act (ACA) coverage expansions, and the aging of the population, drive faster projected growth in health spending in 2014 and beyond.
- Expected growth for 2014 is 5.6 percent, as 9 million Americans are projected to gain health insurance coverage, predominantly through Medicaid or the Health Insurance Marketplaces.
- Average annual projected growth of 6.0 percent per year is projected for 2015 through 2023, largely as a result of the continued implementation of the ACA coverage expansions, faster projected economic growth, and the aging of the population. While projected growth is faster compared to recent experience, it is still slower than the growth observed over the longer-term history.
- The number of uninsured people is expected to decline from 45 million people in 2012 to 23 million people by 2023.
- By 2023, health expenditures financed by federal, state, and local governments are projected to account for 48 percent of national health spending and to reach a total of $2.5 trillion; in 2012, such expenditures constituted 44 percent of national health spending and $1.2 trillion.
- Health spending is projected to be 19.3 percent of GDP by 2023, up from 17.2 percent in 2012.
Major Findings by Payer
Medicare
- Due to a deceleration in growth driven by sequestration and lower utilization across services, Medicare spending growth is projected to have slowed to 3.3 percent in 2013, down from 4.8 percent growth in 2012, and to have totaled $591.2 billion.
- Projected Medicare spending growth of 4.2 percent in 2014 reflects both an expected increase in use and intensity of Medicare services, alongside slow increases in payment rates. For 2015, Medicare growth is projected to slow to 2.7 percent, mostly due to lower payments to Medicare Advantage plans.
- For 2016 through 2023, projected Medicare spending growth is expected to rebound to 7.3 percent per year due to increased enrollment by the baby boomers, increased utilization of care, and higher payment rates driven by improved economic conditions, which increase growth in the cost of input goods and services used to treat Medicarepatients. These drivers in growth will be partially offset by slow growth in payment updates due to provisions in the Affordable Care Act and sequestration.
Medicaid
- Medicaid spending is anticipated to have grown 6.7 percent and to have reached $449.5 billion in 2013, driven by higher payments rates to primary care physicians called for in the Affordable Care Act, as well as actions by states that increased provider reimbursement rates and expanded benefits.
- Total Medicaid spending is projected to grow 12.8 percent in 2014 due to increased enrollment of nearly 8 million beneficiaries. Primarily driving the increase in enrollment are states that chose to expand coverage to adults up to 138 percent of the federal poverty level.
- As some states are expected to expand their Medicaid programs after 2014, an additional 8.5 million people are expected to enroll in the program by 2016. Medicaid spending is expected to grow by 6.7 percent in 2015, and 8.6 percent in 2016. For 2016 to 2023, Medicaid spending growth is projected to be 6.8 percent per year on average.
Private Health Insurance
- Spending for total private health insurance premiums ($947.5 billion) is projected to have grown by 3.3 percent in 2013, or about the same rate of growth as was observed for 2012. Premiums in 2013 are expected to grow slightly faster than benefits (3.0 percent) due to 6.0 percent growth in the net cost of private health insurance, an increase from 0.1 percent growth in 2012.
- Private health insurance premium growth is projected to reach 6.8 percent in 2014 due to higher per enrollee spending and increased enrollment through Marketplace plans.
- Private health insurance spending growth is expected to remain somewhat elevated at 6.9 percent in 2015, primarily due to additional enrollment into health insurance plans. For 2016 through 2023, after the ACA-related enrollment shifts play out, the effects of improved economic conditions are expected to sustain average private health insurance spending growth of 5.4 percent per year.
Out-of-Pocket
- In 2013, out-of-pocket spending is projected to have grown 3.2 percent, slightly slower than the growth rates in 2011 and 2012, and to have reached $338.6 billion. Relatively slow growth in out-of-pocket spending is due to low growth in utilization, and higher cost-sharing requirements for the insured, which tend to discourage people from using covered services.
- Out-of-pocket spending growth is projected to decrease by 0.2 percent in 2014 as a result of the Affordable Care Act’s coverage expansions.
- While out-of-pocket spending growth is projected to accelerate after 2015, reaching a peak of 5.8 percent in 2020, the out-of-pocket share of health spending is projected to fall from 11.7 percent in 2013 to 9.9 percent by 2023.
Major Findings by Sector
Hospital
- Total hospital spending is anticipated to have slowed to 4.1 percent in 2013, reaching $918.8 billion, compared with 4.9 percent growth in 2012. This would represent the fourth consecutive year that hospital spending growth has been under 5 percent after averaging 7.2 percent for 2001 through 2009.
- In 2014, hospital spending growth is projected to be 4.5 percent, which largely reflects greater use of hospital services associated with the coverage expansions from the Affordable Care Act.
- In 2015, hospital spending is projected to increase 5.1 percent due to the continued effects of the ACA insurance expansion combined with the effect of faster economic growth. For 2016 through 2023, continued population aging and the impacts of improved economic conditions are expected to result in projected average annual growth of 6.2 percent.
Physician and Clinical Services
- Growth in spending on physician and clinical services (583.9 billion) is projected to have decelerated in 2013 to 3.3 percent, after growth of 4.6 percent in 2012 (and would mark the fifth consecutive year this rate would be below 5.0 percent). This trend is related to the slowest growth in physician prices since 2002, which is due in part to the sequester and procedural payment changes in Medicare.
- In 2014, physician and clinical services spending growth is projected to be 5.9 percent. As many of the newly insured are anticipated to be generally younger, on average, compared to the current Medicaid and private insurance populations, they are expected to devote a relatively larger share of their medical spending to prescription drugs and physician and clinical services than to hospital care.
- For 2015, lower payments to Medicare Advantage plans, as well as expiration of temporary payment increases to Medicaid providers, is expected to slow growth to 3.8 percent for physician and clinical services.
- For 2016-2023 Medicare spending on physician and clinical services is projected to average 7.1 percent due to more favorable economic conditions and higher enrollment in private health insurance plans.
Prescription Drugs
- In 2013, prescription drug spending is projected to have grown 3.3 percent (reaching $272.1 billion), compared to 0.4 percent growth in 2012. The projected acceleration is due to a smaller descending impact on growth from patent expirations (many of which exerted significant downward pressure on growth in 2011 and 2012) and increased utilization of prescription drugs.
- Projected prescription drug spending growth is 6.8 percent for 2014, and 6.4 percent in 2015, driven by increases in the use of prescription drugs among people who are newly insured and those who move to more generous insurance plans as a result of the premium and cost-sharing subsidies offered by the Affordable Care Act.
- Prescription drug spending is projected to average 5.4 percent for 2016 through 2019 and 6.0 percent for 2020-2023. Faster growth is projected for 2020-2023 due to improving economic conditions, an expected rising trend of expensive specialty drugs being purchased through retail channels, and anticipated changing clinical guidelines designed to encourage drug therapies at earlier stages of treatment.
Major Findings by Sponsor
- Health care spending sponsored (or financed) by federal, state, and local governments is projected to have grown 3.2 percent (to $1.3 trillion) in 2013.
- Reflecting growth trends in private health insurance and out-of-pocket spending, outlays by businesses, households, and other private sources are projected to have risen by 3.9 percent in 2013, compared to 4.6 percent in 2012, and to have reached $1.6 trillion in 2013.
- For 2014, health care financing is projected to shift from households towards the federal government due to features of the Affordable Care Act coverage expansions, such as the 100-percent initial federal matching rate for newly eligible Medicaid enrollees, and subsidies for Marketplace coverage. As a result, the federal government’s share of spending is projected to increase to 28 percent in 2014, from 26 percent in 2013.
- The government-sponsored share of health spending is projected to increase and account for 48 percent of national health expenditures by 2023, largely driven by Medicaid coverage expansions, Marketplace plan premium and cost-sharing subsidies, and an increasing gap between dedicated Medicare financing and program outlays.
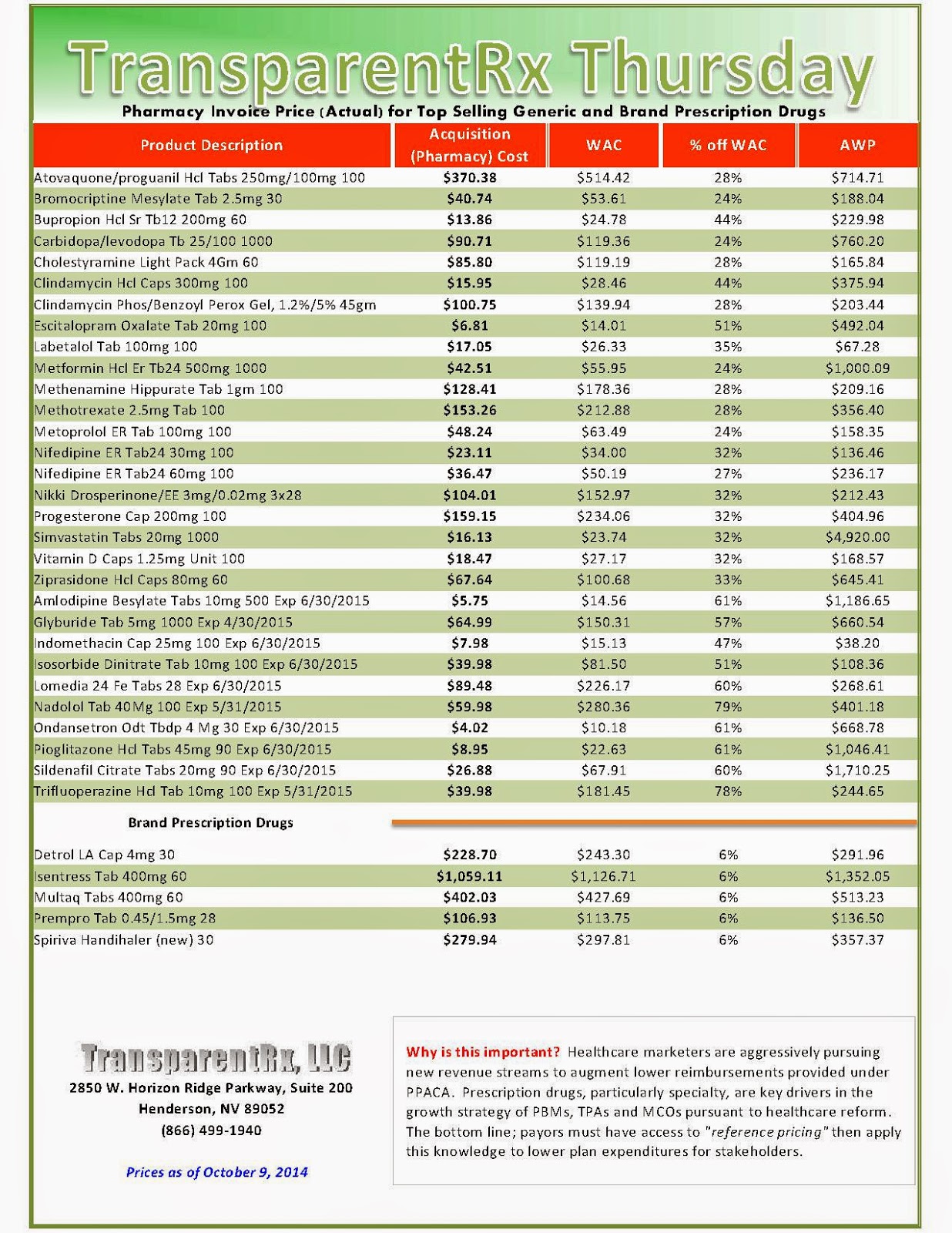
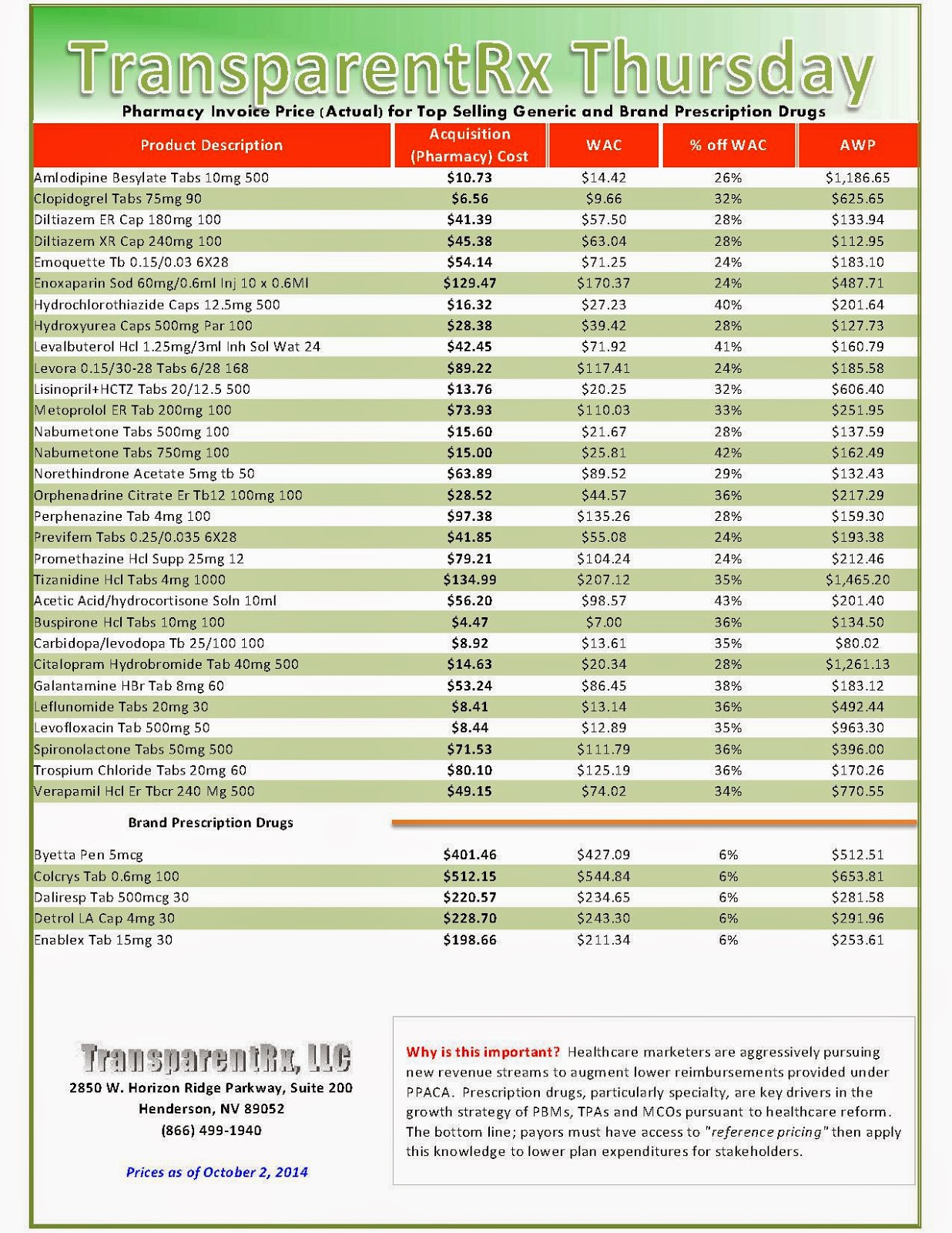
Reference Pricing: Pharmacy Invoice Cost (ACTUAL) for Top Selling Generic and Brand Prescription Drugs
The costs shared below are what our pharmacy actually pays; not AWP, MAC or WAC. The bottom line; payers must have access to “reference pricing.” Apply this knowledge to hold PBMs accountable and lower plan expenditures for stakeholders.
| How to Determine if Your Company [or Client] is Overpaying |
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our pharmacy cost then determine if a problem exists. When there is a 5% or more price differential (paid versus actual cost) we consider this a problem.
When better pricing is discovered the contract language should stipulate the client be indemnified. Do not allow the PBM to limit the market check language to a similar size client, benefit design and/or drug utilization. In this case, the market check language is effectually meaningless.
Click here to register: “How To Slash the Cost of Your PBM Service, up to 50%, Without Changing Providers or Employee Benefit Levels.” [Free Webinar]
Generic Drug Field Full of Pricing Traps
*********************************************************************************
A friend of mine, a diabetic, stumbled on to another booby trap in the pricing of generic drugs. In my last column I described the new two-tiered arrangements insurers are pushing on patients. You can choose a non-preferred generic and pay more, maybe a lot more, or a preferred generic and get a price break. That’s the same pricing scheme insurers use for the expensive brand-name drugs.
 |
| Rising costs are a direct result of demand |
Consumer groups, doctors, and insurance carriers have encouraged patients to choose generics over the name brands as a way to help lower the nation’s healthcare tab. So for many years my friend has been using a generic drug called Gemfibrozil that diabetics often take to lower triglycerides and cholesterol.
It has worked for him. No nasty drug interactions. No nasty side effects. And the price has been low–$2.71 for 60 pills. In August the price more than doubled to $6.14. He was still OK with that.
He was not OK when he got a bill in September from Express Scripts, the pharmacy benefit manager for his Medigap carrier whose plan is offered by his former employer, the City of New York. (PBMs, as they’re called, manage the drug benefits for employers and insurers and supposedly help hold the line on prices.)
Express Scripts wrote his doctor without consulting my friend, the patient, suggesting that for reasons of “safety and efficacy,” he should switch his patient to a different drug, a generic called Fenofibric acid. His share of the cost would now be $156.70 for 90 pills. Fenofibric acid costs $1.74 per pill compared to Gemfibrozil’s 10 cents a pill resulting in an out-of-pocket cost increase of 1,640 percent.
Why the switch, my friend asked his doctor. The doctor pointed to the reasons given in the letter about an increased risk of skeletal muscle effects and said maybe it was advisable to try the new drug. He was, however, astounded by the price, but my friend said it was clear the doctor wasn’t going to fight the PBM.
My friend spoke to an official at New York City’s employee benefits office who said her office has never heard of a PBM recommending that a more expensive generic drug replace a cheaper one.
I rang up John Rother, former chief lobbyist for AARP and now head of a group called the National Coalition on Health Care. The Coalition is waging a campaign to educate the public about the exorbitant prices of drugs, particularly the Hepatitis C drug Sovaldi and other specialty drugs in the pipeline that will carry super high price tags.
“Generic drug prices have been rising steeply, and there doesn’t seem to be an explanation for it,” Rother told me. He said he could only guess that some generic drug makers are leaving the market and the ones remaining will have less competition and the power to increase market share and raise prices.
Maybe there are medical reasons my friend should make the switch, but so far his doctor hasn’t been persuasive. Has the PBM discovered new side effects for the drug he’s been taking? Who’s treating the patient—the doctor or the PBM? And how does this big price jump fit in with the PBM’s purported mission: to save money for insurers and employers? Was my friend caught in a tussle between the clinician and the bean counters? How does he know who’s right without doing extensive research himself?
Since individuals can’t negotiate prices with drug companies, and Congress has prohibited Medicare from negotiating prices when it passed the prescription drug benefit law in 2003, my friend says, “companies have carte blanche to rip people off. In situations like this no one ever talks straight, but someone is making a lot more money.” He’s trying to get back on Gemfibrozil or a similar generic that’s cheaper than the one the PBM suggested.
Rother looks at the big picture now coming into focus from the sharply rising prices of generics. “Four years after we passed what we thought was universal health coverage, you can’t get the medicines you need because of the prices. It’s tragic,” he says.
By Trudy Lieberman, Rural Health News Service
Click here to register: “How To Slash the Cost of Your PBM Service, up to 50%, Without Changing Providers or Employee Benefit Levels.” [Free Webinar]
Reference Pricing: Pharmacy Invoice Cost (ACTUAL) for Top Selling Generic and Brand Prescription Drugs
The costs shared below are what our pharmacy actually pays; not AWP, MAC or WAC. The bottom line; payers must have access to “reference pricing.” Apply this knowledge to hold PBMs accountable and lower plan expenditures for stakeholders.
| How to Determine if Your Company [or Client] is Overpaying |
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our pharmacy cost then determine if a problem exists. When there is a 5% or more price differential (paid versus actual cost) we consider this a problem.
When better pricing is discovered the contract language should stipulate the client be indemnified. Do not allow the PBM to limit the market check language to a similar size client, benefit design and/or drug utilization. In this case, the market check language is effectually meaningless.
Click here to register: “How To Slash the Cost of Your PBM Service, up to 50%, Without Changing Providers or Employee Benefit Levels.” [Free Webinar]
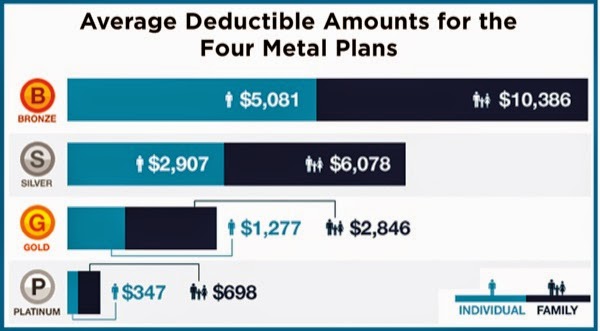
Can Specialty Pharmacies Ease the Pain Of Soaring Deductibles?
In 2013, Ms. Potter noted, 17% of employers offered high-deductible health plans as their employees’ only option—up 31% from 2012, according to PricewaterhouseCoopers’ “Behind the Numbers 2014.” For 2014, she said, some 44% of employers were considering such a move (http://pwc.to/1eRYLxr).
High-deductible plans can pose challenges for anyone with a chronic condition, but they are particularly problematic for patients taking expensive specialty medications, with annual minimum deductibles of $1,250 per person and $2,500 per family. The 2014 annual cap on out-of-pocket costs is $6,350 for an individual and $12,700 for a family—high for anyone, but harder to swallow if it’s front-loaded into the first month or two of each year because of costly specialty drugs.
Those steep costs can be a powerful trigger for noncompliance. In one study, high-deductible health plans were found to reduce adherence to prescription medication regimens in four of five conditions evaluated: hypertension, dyslipidemia, diabetes and depression (Am J Managed Care 2013;19:e400-e407), Ms. Potter noted. Only in asthma/chronic obstructive pulmonary disease was there not a significant decline in adherence.
The conditions included in the compliance study generally do not require specialty medications, Ms. Potter pointed out; it’s thus possible that the documented adherence problems might be even more pronounced when it comes to specialty medications, “particularly because few of these drugs have generic alternatives in a lower tier, and patients may have to pay $7,600 or more per year out of pocket for specialty medications,” she said.
Health Exchanges Not Immune
If employer-sponsored plans are increasingly moving toward high deductibles, many plans on the new health insurance exchanges—especially at the lower bronze “metal level”—are already there. In December, HealthPocket Inc., which compares health insurance plans for consumers, found that the average annual individual deductible for a bronze plan was just over $5,000, in addition to the average premium of $295.51 a month, or $3,546 a year (http://bit.ly/1oevFqq).
“These high-deductible plans are causing a bit of a problem,” Debbie Stern, president of Rxperts, told Specialty Pharmacy Continuum. “It’s really putting a high burden on the patient to come up with all of that up front. Even if it’s just a $2,000 deductible, the patient has to pay that up front almost immediately for most specialty drugs, so the first prescription is going to cost them almost the full out-of-pocket for the year. When these plans were designed, people were thinking of drugs that cost $200 a month, not specialty drugs that cost $2,000 a month or more.”
Here’s where good specialty pharmacies can really distinguish themselves, Ms. Potter said. “You can provide additional patient support, working proactively to help patients understand their medical plans and anticipate their financial demands.” (See sidebar for more details on these strategies.)
That’s already happening at many specialty pharmacies around the country, according to Kyle Skiermont, PharmD, the director of specialty/infusion operations at Fairview Pharmacy Services in Minneapolis. “We’re seeing a big increase in high-deductible plans, along with a rise of coinsurance,” Dr. Skiermont said. “We’re seeing both more patients with these plans, as well as higher dollar amounts they’re needing.”
Fairview has doubled its staff of patient financial advocates over the past year to help address the growing need. And it’s not just that more patients need assistance—their situations are also becoming more and more complicated, Dr. Skiermont noted. “Where one advocate might have been able to handle many more patients in the past,” he said, “each patient we are helping is taking more time and getting more complex in [his or her] needs.”
Many of the foundations and other sources of funding for medication assistance are also getting tapped out more quickly. That, too, requires creativity. “Some foundations recharge their funds over the year, so if you ask for a grant on behalf of your patient and it’s not there, you need to know when to go back to them,” Dr. Skiermont said. “Maybe there was no funding in March but there may be in October. It requires a lot more interaction and advocacy for our patients, multiple times a year, whereas historically we might have only needed to do that once a year.”
“We’ve been getting more and more creative around what we can do as far as payment plans,” Dr. Skiermont added. “If we know someone has a big out-of-pocket maximum that they’re going to hit in the first month, we’ll try to make arrangements to pay that over the year.”
It’s a patchwork solution that likely is not sustainable in the long term. “In the short term, we feel we owe this to our patients. As a nonprofit, health-system–based specialty pharmacy, providing this kind of high-touch financial assistance is one of our differentiators.
It’s core to our mission,” Dr. Skiermont said. “We need to continue to be innovative and make this work for our patients, but ultimately something is going to have to change. A lot of the burden is falling on specialty pharmacy, but at the same time, the providers and the pharmaceutical companies are beginning to understand the coverage issues better than they did a couple of years ago, and are helping us bring the message to the patient. The reality is that everyone’s still trying to figure this out.”
by Gina Shaw
Reference Pricing: Pharmacy Invoice Cost (ACTUAL) for Top Selling Generic and Brand Prescription Drugs
The costs shared below are what our pharmacy actually pays; not AWP, MAC or WAC. The bottom line; payers must have access to “reference pricing.” Apply this knowledge to hold PBMs accountable and lower plan expenditures for stakeholders.
| How to Determine if Your Company [or Client] is Overpaying |
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our pharmacy cost then determine if a problem exists. When there is a 5% or more price differential (paid versus actual cost) we consider this a problem.
When better pricing is discovered the contract language should stipulate the client be indemnified. Do not allow the PBM to limit the market check language to a similar size client, benefit design and/or drug utilization. In this case, the market check language is effectually meaningless.
Click here to register: “How To Slash the Cost of Your PBM Service, up to 50%, Without Changing Providers or Employee Benefit Levels.” [Free Webinar]
States step in to regulate drug copays
 At least five states have enacted laws limiting copays and two — New York and Alaska — have expressly prohibited the use of tiered formularies for specialty medications. Another 11 states, including California, Illinois and Virginia, have legislation up for consideration that would limit copays.
At least five states have enacted laws limiting copays and two — New York and Alaska — have expressly prohibited the use of tiered formularies for specialty medications. Another 11 states, including California, Illinois and Virginia, have legislation up for consideration that would limit copays.
That state governments are stepping in to place limits on cost-sharing for specialty drugs suggests that public angst over rising out-of-pocket costs is reaching an inflection point—monthly drug costs that were once affordable for patients with conditions like arthritis or multiple sclerosis are becoming harder to cover as part of a family budget. Consumers are seeking relief and lawmakers are turning to insurers to limit what they can charge their members.
“The trend towards increased reliance on specialty pharmaceuticals would not raise such an important concern if specialty drugs did not represent the most expensive segment of pharmaceuticals not only for insurers, but also for consumers through cost-sharing measures,” as Chad Brooker, a health policy analyst at Connecticut’s insurance exchange, Access Health, wrote in Health Law and Policy Brief last year.
By some estimates, specialty medications account for only one percent of all U.S. prescriptions but 25 percent of national drug spending. Not only is that set to grow to as much as 45 percent by 2017, but the assumption that prices for existing will fall over time may not always be the norm.
Teva Pharmaceuticals’ Copaxone, an injection-based multiple sclerosis drug, debuted in 1996 at a price of about $1,000 per month, by 2008 was priced at $2,000 per month, and nowadays is hovering around $5,000. To continue reading click here.
By: Anthony Brino
Click here to register for: “How To Slash the Cost of Your PBM Service, up to 50%, Without Changing Providers or Employee Benefit Levels.” [Free Webinar]
Reference Pricing: Pharmacy Invoice Cost (ACTUAL) for Top Selling Generic and Brand Prescription Drugs
The costs shared below are what our pharmacy actually pays; not AWP, MAC or WAC. The bottom line; payers must have access to “reference pricing.” Apply this knowledge to hold PBMs accountable and lower plan expenditures for stakeholders.
| How to Determine if Your Company [or Client] is Overpaying |
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our pharmacy cost then determine if a problem exists. When there is a 5% or more price differential (paid versus actual cost) we consider this a problem.
When better pricing is discovered the contract language should stipulate the client be indemnified. Do not allow the PBM to limit the market check language to a similar size client, benefit design and/or drug utilization. In this case, the market check language is effectually meaningless.
Click here to register: “How To Slash the Cost of Your PBM Service, up to 50%, Without Changing Providers or Employee Benefit Levels.” [Free Webinar]
_1.jpg)

_1.jpg)
_1.jpg)
_1.jpg)
_1.jpg)