Employer Coverage of GLP-1 Drugs Jumps [Weekly Roundup]
Employer Coverage of GLP-1 Drugs Jumps and other notes from around the interweb:
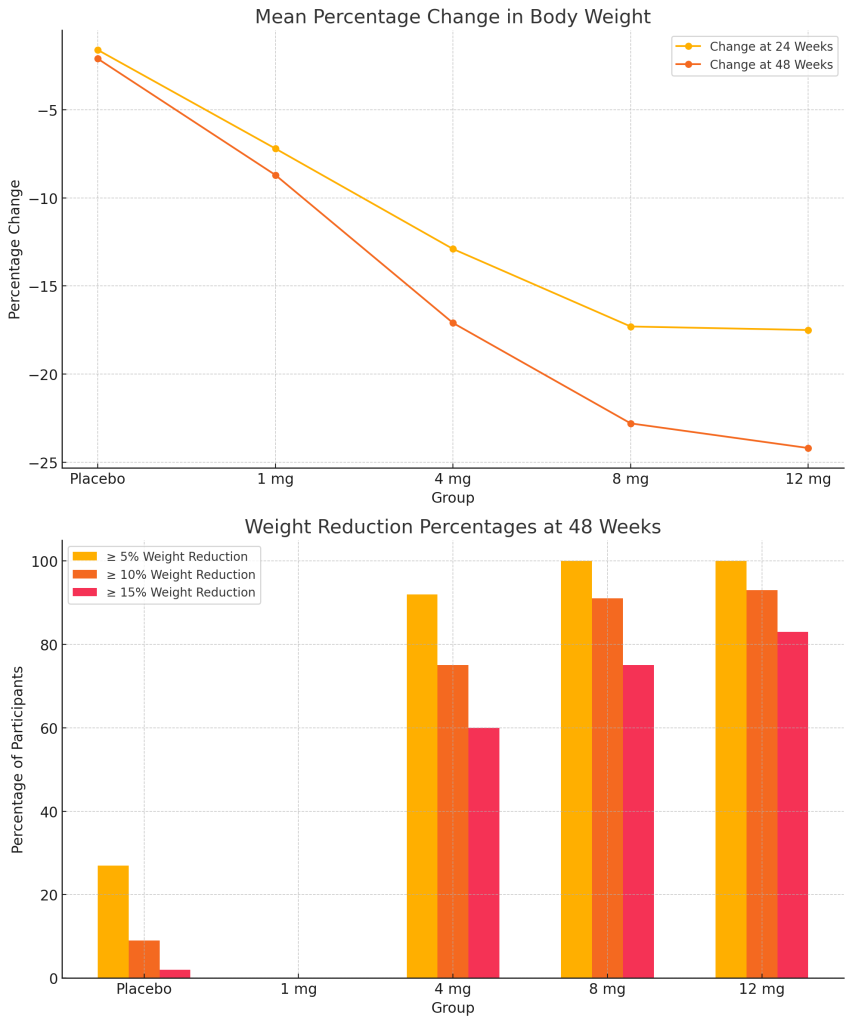
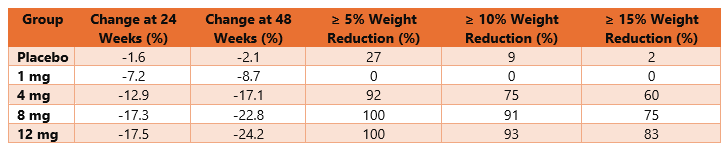
- Employer Coverage of GLP-1 Drugs Jumps. As the popularity of GLP-1 drugs like Ozempic and Wegovy grows, so does the percentage of employers covering the drugs for employees. A new employer survey out June 13 from the International Foundation of Employee Benefit Plans (IFEBP) found that employer coverage of the drugs is up 8 percentage points since last fall, with roughly one-third of companies now offering GLP-1 drug coverage for both diabetes management and weight loss. More than half of employers (57%) currently provide coverage for diabetes only—the original intended use for the drugs—up from 49% in 2023. Perhaps even more significant, 34% provide coverage for both diabetes and weight loss (up from 26% in 2023), according to the benefits organization’s May survey of 279 employers. IFEBP, which counts some 31,000 organizations as members, last surveyed employers abut GLP-1 drugs in October 2023. It’s a big jump that shows employers are getting serious about coverage of the drugs, especially as employees express interest, said Julie Stich, vice president of content at IFEBP.
- Mail-Order Drugs Were Supposed to Keep Costs Down. One employer was paying about $100 for a prescription for a generic antidepressant, though it could be bought elsewhere for about $12. A key tool that businesses have counted on to keep a lid on employees’ drug spending—filling workers’ prescriptions by mail—is now driving up their costs. Unity Care NW, a nonprofit health clinic in Washington state, forecasts the cost of medical and drug benefits for its 365 employees and their family members will increase this year by 25% to more than $3 million. A big reason: Drugs delivered by mail are costing multiples more than those picked up at a store counter. Markups were as much as 35 times higher than what other pharmacies charged, according to a recent analysis of millions of prescriptions in Washington state. The stakes nationally are huge, in a medical market with escalating prescription prices and increasing concentration of medical providers in direct employment by hospital groups.
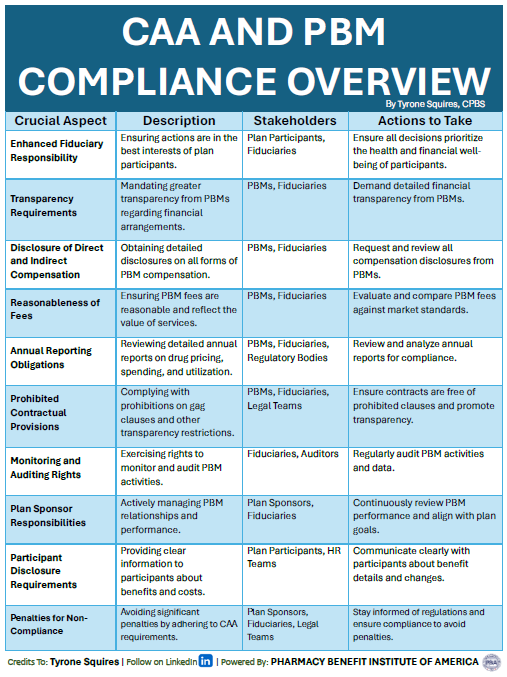
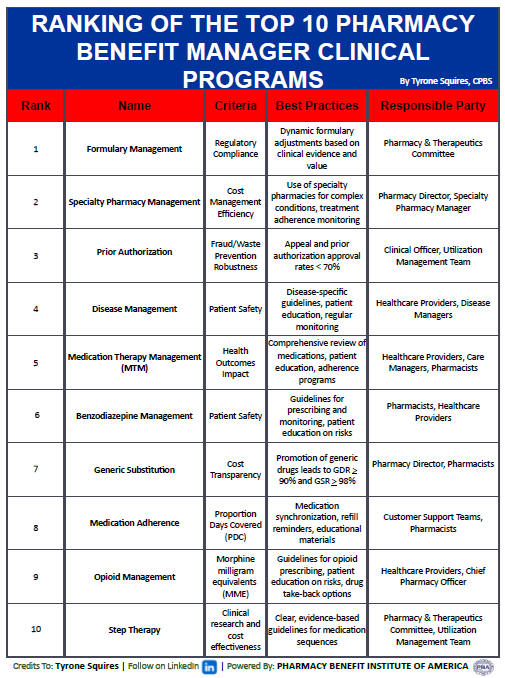
- The J&J lawsuit should be a wakeup call to the PBM industry — and to companies everywhere. The ongoing legal dispute involving Johnson & Johnson has again thrust the topic of pharmacy benefit managers (PBMs) into the spotlight. Ann Lewandowski, a J&J employee, sued the company for overpaying for its employees’ prescription drugs through its PBM, Express Scripts, claiming that these overpayments resulted in higher health insurance premiums and out-of-pocket drug costs for employees. This lawsuit is a significant entrant in the recent groundswell of efforts to shine light on the traditional PBM industry and its opaque pricing structures and outdated evaluation models. It follows on the heels of probes by government regulators and attention from Congress into PBMs’ business practices. In late May, executives from three major PBMs were asked to testify before the House Committee on Oversight and Accountability.
- Mark Cuban’s D2C pharmacy won’t beat most insured patients’ out of pocket drug prices, one study finds. Insured patients are often better off buying their generic prescriptions through their health insurance benefits than through Mark Cuban Cost Plus Drug Company, though those without insurance could find cost savings in over a quarter of their pharmacy fills, according to a study published Friday in JAMA Health Forum. Across a sample of nearly 844 million prescription pharmacy fills logged among 124 generic drugs in 2019, researchers found that nearly 100 million (11.8%) would have reduced out-of-pocket spending for patients if they had been acquired through the billionaire-backed manufacturer and distributor. Cost Plus Drugs’ direct-to-consumer pharmacy didn’t launch until 2022. To measure the company’s hypothetical savings for consumers at the individual level, researchers adjusted the per-drug out-of-pocket costs from their sample based on the Center for Medicare and Medicaid Services’ 2023 National Average Drug Acquisition Cost.