3 Digital Health Strategies to Improve Health Plan Member Experience [Weekly Roundup]
3 Digital Health Strategies to Improve Health Plan Member Experience and other notes from around the interweb:
- 3 Digital Health Strategies to Improve Health Plan Member Experience. Health plans have innumerable reasons to focus on improving member experience right now. The Centers for Medicare and Medicaid Services (CMS) are heavily weighting member experience in STARS ratings and HEDIS scores. And healthcare consumers want more accessible care and support. Digital member engagement tools give health plans the opportunity to deliver a better member experience by making healthcare more convenient—which, in turn, drives satisfaction and retention. Members are also looking to get the best value for the soaring prices they’re paying for health insurance coverage. But adopting a new digital health solution can be challenging, especially when it comes to aligning goals with staff and member expectations. Building a digital engagement strategy requires buy-in from individuals across an organization. Here, we’re highlighting three strategies health plans can use to improve digital adoption and enhance the member experience.
- 15 biggest pharmacies by prescription revenue. Pharmacies earned a record $548 billion from prescription dispensing revenues in 2022, and 15 pharmacies account for 75 percent of that figure, according to Drug Channels. The market share from the top fifteen dipped from 2020 to 2021 and again from 2021 to 2022, according to past reports. They accounted for 78.6 percent of the market in 2020, 76.9 percent in 2021 and 75.6 percent in 2022, according to the site’s past reports. The decrease from 2021 to 2022 is because of Walgreens’ losses after the Prime Therapeutics deal, the report said. Five of the largest pharmaceutical companies are owned by companies that also have a pharmacy benefit manager, including CVS with Caremark, Cigna with Express Scripts, Centene with Envolve Health, Humana with CenterWell and UnitedHealth Group with Optum. Click here to see the Top 15 ranked by prescription revenue.
- Survey: More than Half of Payers Use Outcomes-based Contracts. About 58% of payers had at least one outcomes-based contract with a pharmacy benefit manager for prescription drugs in 2022, according to a survey published last week. In an outcomes-based contract, prescription drug reimbursement is based on the outcomes achieved for the patient. These contracts represent a shift to value-based care. Avalere Health, a healthcare business consulting firm, published the survey. The company conducted it online from February 14 to February 20 and received responses from forty-six health plans. This is the fifth year the company has conducted the survey. Of the payers that had at least one outcomes-based contract, more than 35% had more than ten outcomes-based contracts in 2022. Another 10% of payers had five to ten contracts, and a little over 10% had two to five contracts. About 15% had no contracts but were in negotiations for one or more. Less than 10% had no contracts and were not planning to take any on. In addition, the survey found that of the respondents who had at least one outcomes-based contract in 2022, the top therapeutic areas the contracts were used for were oncology, cardiology, endocrinology. The therapeutic areas with the lowest number of outcomes-based contracts were infectious disease, pulmonology, and rheumatology.
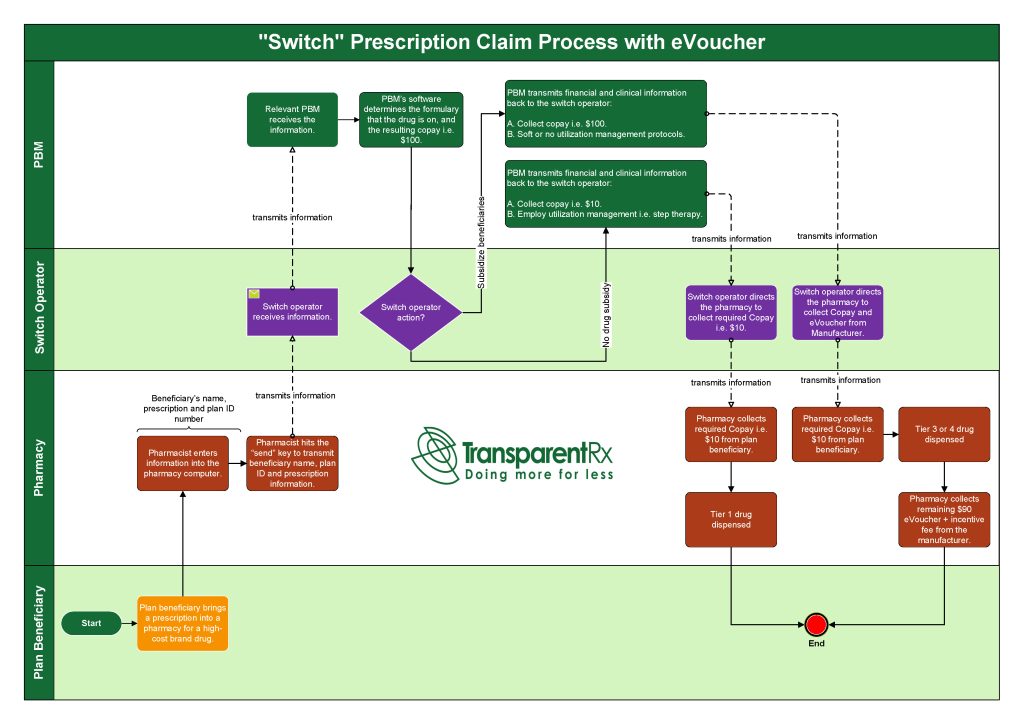
- What is transparency? Six things to look for in a PBM contract. If you don’t know the answer, they’re not transparent. PBMs aren’t incentivized to be transparent because they make money on drugs in many creative ways. So long as this remains true, their interests are not aligned with those of the employer or employees, and being transparent puts their business model at risk. For example, it’s an open secret that many PBMs make huge profits by negotiating “rebates” with drug manufacturers in the name of lowering the price of drugs. The truth is that those PBMs run a pay-to-play scheme, excluding from their formularies the drug manufacturers that don’t pay the rebates. The PBMs argue they are now passing most rebates received to employers to reduce drug costs. It should be no surprise that, at the same time rebate revenue has gone down for PBMs, they experienced a commensurate or greater increase in “admin fees” received from manufacturers for “processing rebates.” Whether you call it a rebate or an admin fee, it has the same effect: driving up wholesale drug prices and lining the PBM’s pocket at employer and patient expense. Another customary practice is “spread pricing,” where a PBM adds margin to the price they pay the pharmacy versus what they charge health plans and patients. Who keeps the spread? The PBMs, of course. And pharmacy owners, health plans, and health care consumers pay the price.