Anthem, Express Scripts largest customer, will not renew its contract with the pharmacy benefit manager
The customer, Anthem — owner of a variety of Blue Cross Blue Shield health insurance firms — is responsible for roughly 18% of Express Scripts’ first quarter revenue, Express Scripts said in a release.
 |
| Click to learn more |
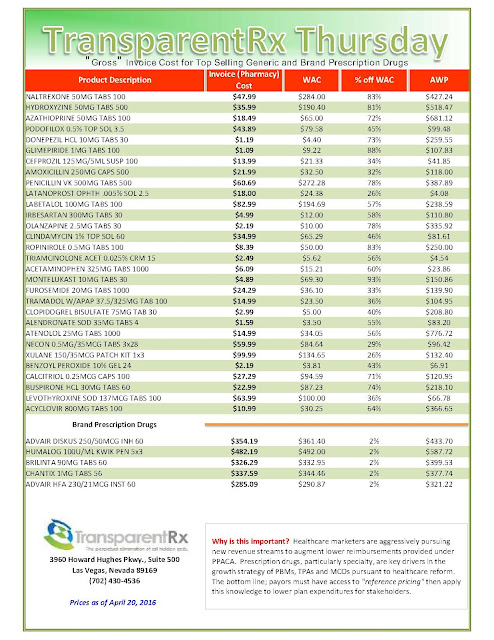
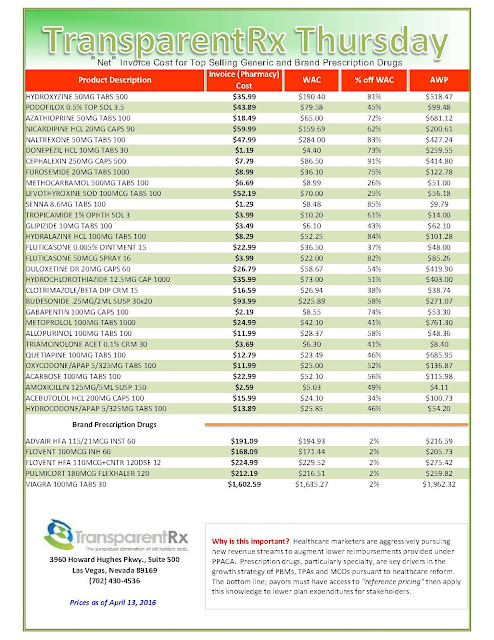
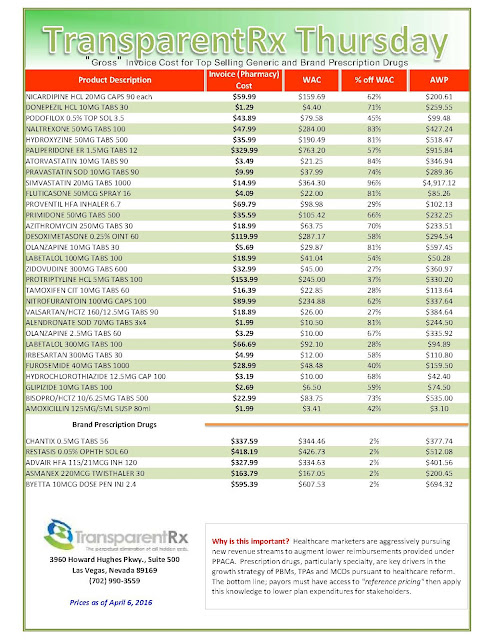
As a health insurer, Anthem contracts with pharmacy benefit managers like Express Scripts to help negotiate lower prices for prescription drugs. Anthem accused Express Scripts of not passing along those savings, claiming Express Scripts overcharged the insurer by billions of dollars. The ending of the contract comes after Anthem last year sued Express Scripts over the issue.
“Although conversations have been ongoing, the Company was recently told by Anthem management that Anthem intends to move its business when the Company’s current contract with Anthem expires on December 31, 2019, and that Anthem is not interested in continuing discussions regarding pricing concessions for 2017-2019 or in receiving the Company’s proposed pricing for the period beyond 2019,” said the release from Express Scripts.
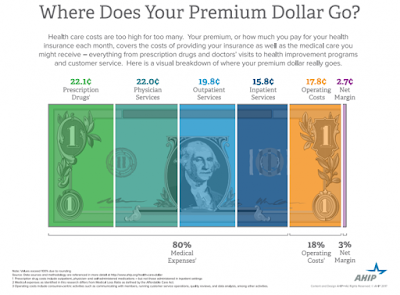
Pharmacy benefit managers, or PBMs, including Express Scripts have come into the spotlight as the drug industry faces increased scrutiny over the price of prescription medicines. Drug companies, which bear the brunt of the heat over this, have been trying to convince people that they’re not the problem. Instead, they’ve pointed the finger at the PBM’s which they say are responsible for negotiating lower prices in the form of rebates.
Those rebates are meant to be passed on to patients, but a recent report from the drug companies’ lobby found that that’s not the case for 20% of prescriptions filled. Instead, the implication here is that the companies meant to pass along the rebates are keeping all of the money for themselves, in those cases. It’s led to finger-pointing from both PBMs and drugmakers over where those rebates are going.