[Free Webinar] The Untold Truth: How Pharmacy Benefit Managers Make Money
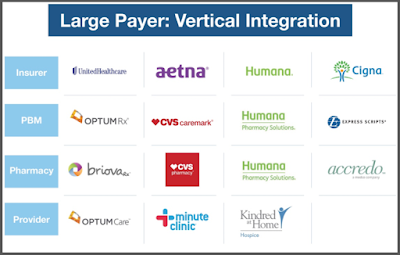
How many businesses do you know want to cut their revenues in half? That’s why traditional pharmacy benefit managers don’t offer a fiduciary standard and instead opt for hidden cash flow opportunities such as rebate masking. Want to learn more?
 “Thank you Tyrone. Nice job, good information.” David Stoots, AVP
“Thank you Tyrone. Nice job, good information.” David Stoots, AVP
A snapshot of what you will learn during this 30 minute webinar:
- Hidden cash flows in the PBM Industry
- Basic to intermediate level PBM terminologies
- Specialty pharmacy cost-containment strategies
- Examples of drugs that you might be covering that are costing you
- The #1 metric to measure when evaluating PBM proposals
TransparentRx
Tyrone D. Squires, MBA
10845 Griffith Peak Drive, Suite 200
Las Vegas, NV 89135
Office: (866) 499-1940
Mobile: (702) 803-4154