How PBMs Make Money and What To Do About It [On-Demand Video]
Prescription drug spending exceeds 400 billion dollars annually and PBMs have a hand in almost every dollar. How PBMs make money is an important consideration for plan sponsors. PBMs offer a valuable service, one which provides pharmacy benefits to nearly 225 million Americans. Unfortunately, very few people outside of the industry understand what they [we] do or how they make money. I aim to put an end to this now.
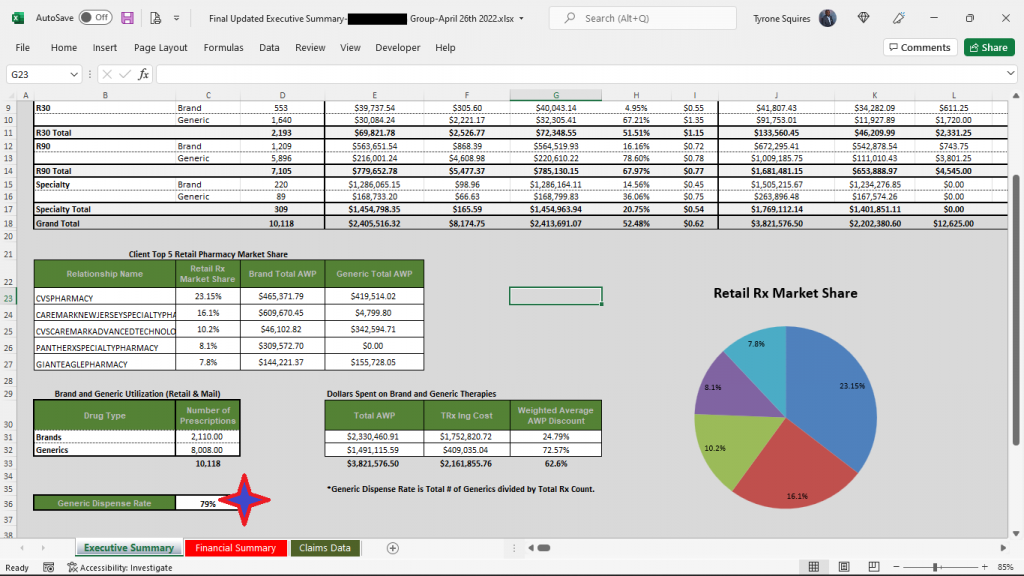
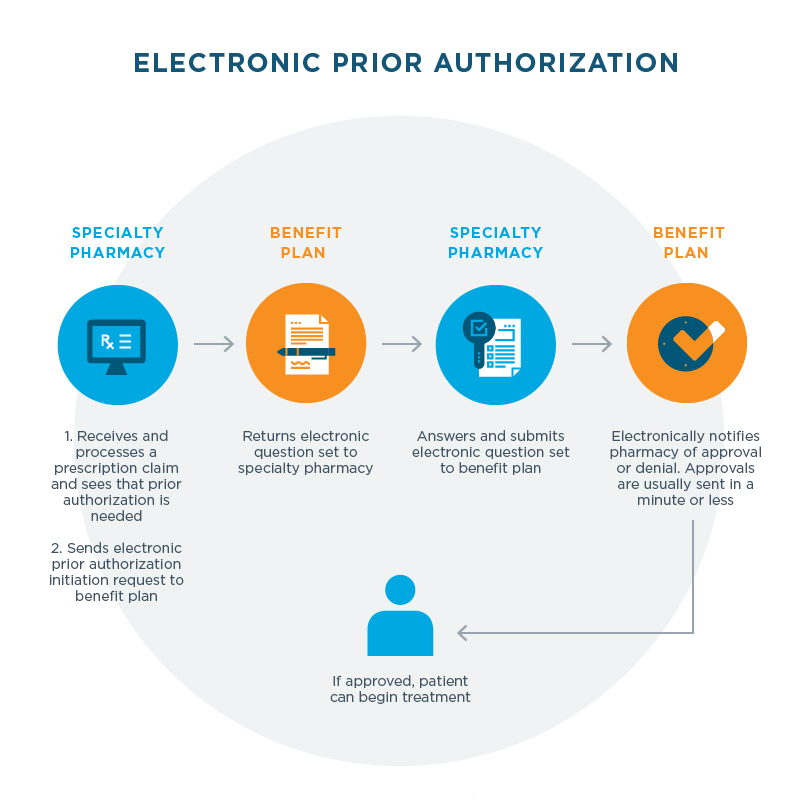
Clients of a PBM include but are not limited to self-funded employers, insurers, managed care organizations, state, and federal government agencies. The client works with the PBM to decide the pharmacy benefit that it will offer, including the drugs that will be covered, the beneficiary’s cost sharing requirements, and the pharmacy network. The client then retains the PBM to administer the pharmacy benefit for its members or employees.
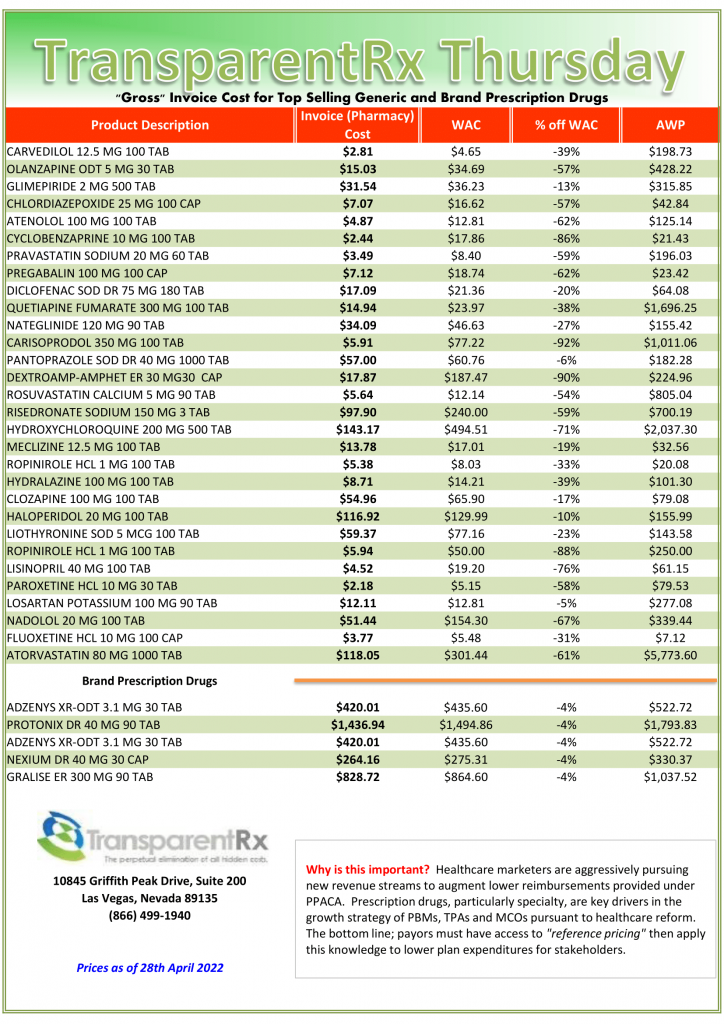
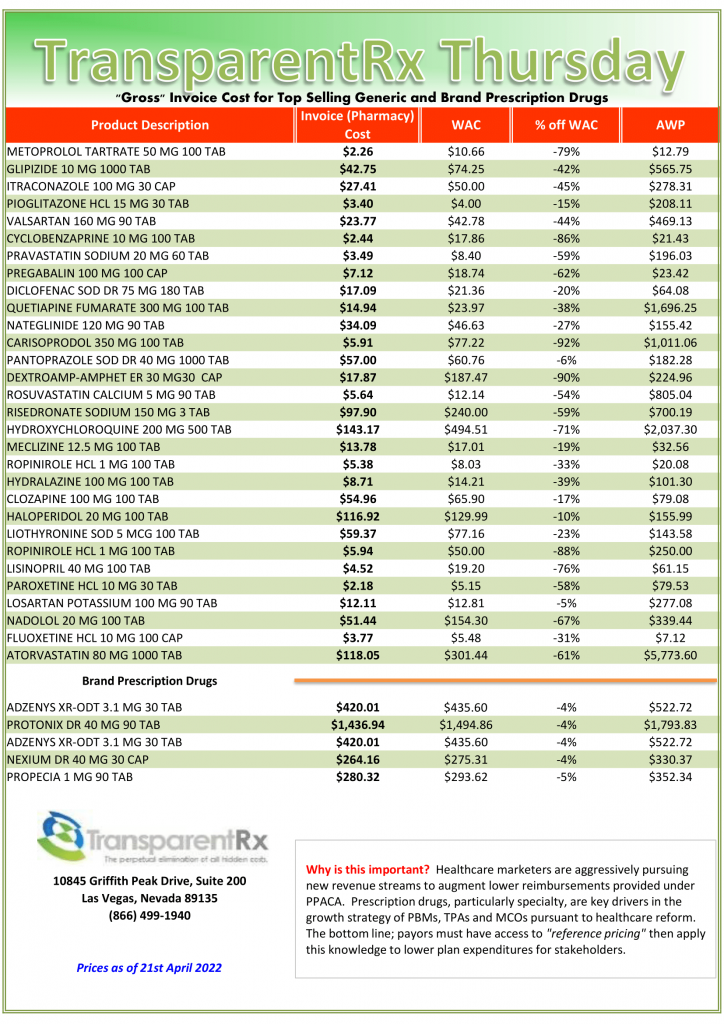
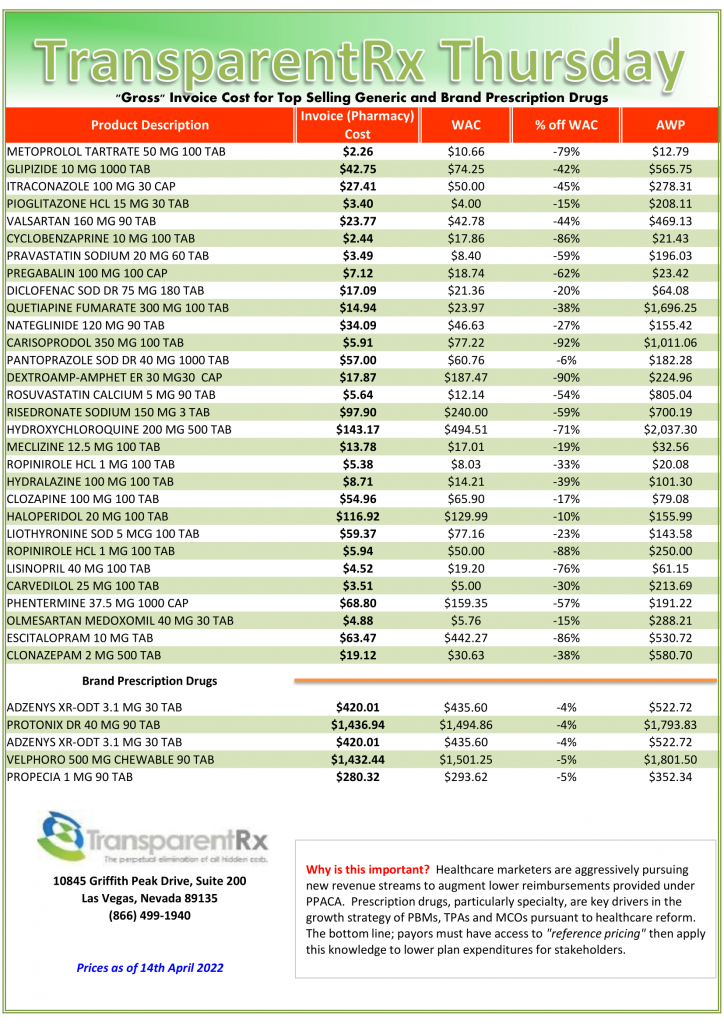
One of the primary reasons clients retain PBMs is that PBMs reduce the cost of offering a pharmacy benefit. PBMs do this in a variety of ways: automating administrative services, negotiating discounts on ingredient cost (drugs), and managing drug utilization. May I speak frankly? Industry catch phrases such as “transparency” and “pass-through pricing” or related words are in my experience half-truths. Demand an airtight fiduciary contract and reference pricing, which includes acquisitions costs and NDCs, from an independent third party to maximize value in every single penny of your pharmacy spend.
Often overlooked, in far too many PBM contracts, is how much cash the PBM generates for itself, on a per client basis. I have a simple equation that every consultant, broker and benefits expert should employ to calculate PBM service costs, but few do. Here it is absence of charge. Is it unreasonable to know exactly how much money your PBM is pocketing for the services it provides to your organization? A non-fiduciary PBM will bark at this notion. In other words, no matter how tight you believe your contract to be a non-fiduciary PBM will find a means to reap excessive revenue from clueless payers unless of course you continue reading. To learn more, watch How PBMs Make Money.