Price is Not Cost: Understanding the Real Drivers Behind Pharmacy Benefit Expenses
In the realm of pharmacy benefit management (PBM), grasping the full scope of costs is crucial for Directors of Benefits and CFOs who strive to optimize their healthcare investments. It’s essential to recognize that the “price” of drugs is not synonymous with “cost.” True cost management requires a nuanced understanding of four primary cost drivers: price, product mix, utilization, and cost share. Let’s delve into each of these components to provide a clearer strategy for managing pharmacy benefits effectively.
Price
Definition: The price is the amount paid for a drug to the manufacturer or pharmacy after accounting for rebates and discounts.
Components:
- List Price: Manufacturer’s initial price for the drug.
- Net Price: Actual price paid after subtracting rebates and discounts provided by manufacturers to payers and PBMs.
- Markup: Additional costs added by pharmacies or PBMs.
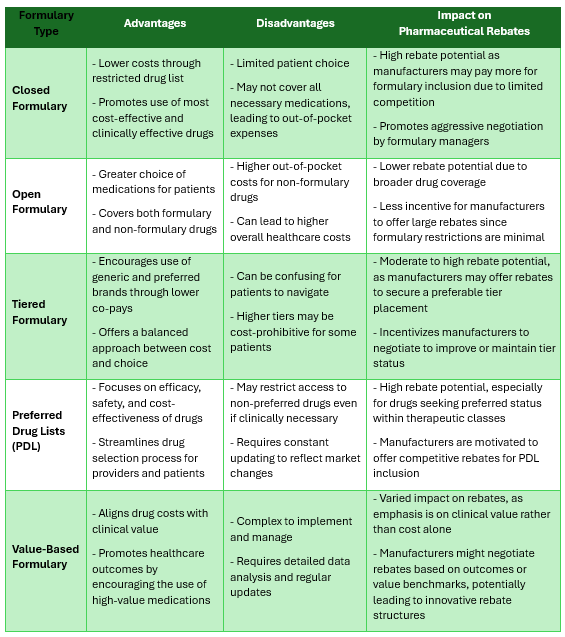
Effective strategies to manage drug prices include negotiating better rebate terms, choosing generics or biosimilars where appropriate, and leveraging competitive bids for PBM contracts.
Product Mix
Definition: Product mix refers to the composition of prescription drugs dispensed under a benefit plan.
Components:
- Generic Dispense Rate (GDR): The proportion of all dispensed prescriptions that are generics, which are typically cheaper than brand-name drugs, should be 88% or higher. Every 1% increase in GDR leads to 5% gross cost savings.
- Therapeutic Alternatives: Use of clinically equivalent drugs that vary in price.
- High-cost Drugs: Biologics and specialty drugs that significantly impact overall spending.
Strategies for optimizing the product mix involve increasing the generic dispensing rate, formulary management to encourage the use of cost-effective therapeutic alternatives and implementing step therapy policies, for example.
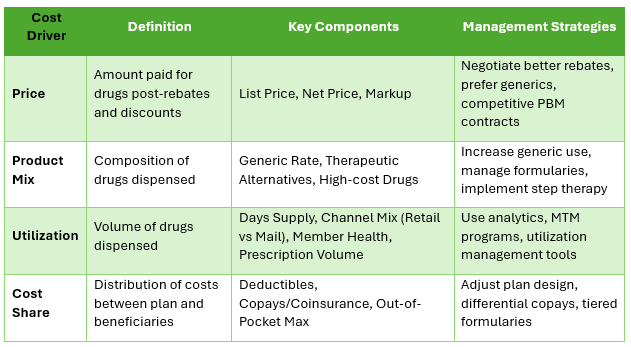
Utilization
Definition: Utilization measures the volume or frequency of drug dispensation under a health plan.
Components:
- Prescription Volume: Total number of prescriptions filled.
- Days Supply: Prescribed amount and the length of time for which a drug is dispensed.
- Member Population Health: The overall health demographics of the covered population which influences disease prevalence and drug usage.
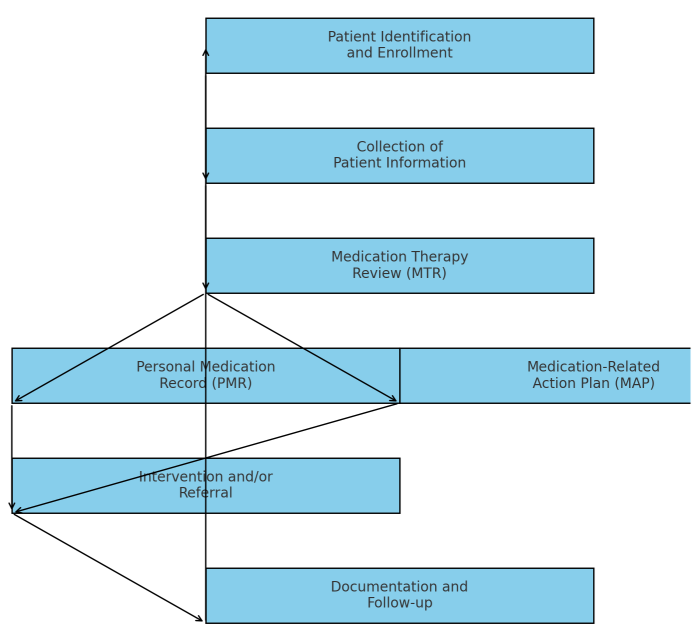
Managing utilization entails using data analytics to forecast trends, implementing medication therapy management (MTM) programs to mitigate risk, and employing utilization management tools like prior authorization. Prior authorization approval rates are lower than 70% for efficient pharmacy benefit management programs.
Cost Share
Definition: Cost share refers to the distribution of drug expenses between the insurance plan and its beneficiaries.
Components:
- Deductibles: The amount a beneficiary must pay out-of-pocket before the health plan starts paying.
- Copayments and Coinsurance: Fixed amounts or percentages of the prescription cost that a beneficiary is responsible for after meeting their deductible.
- Out-of-Pocket Maximums: The maximum amount a beneficiary pays in a year, after which the plan covers 100% of additional costs.
To optimize cost sharing, strategies include adjusting plan design to influence drug choices through differential copays for generics versus brands and using tiered formularies to incentivize lower-cost options.
Conclusion
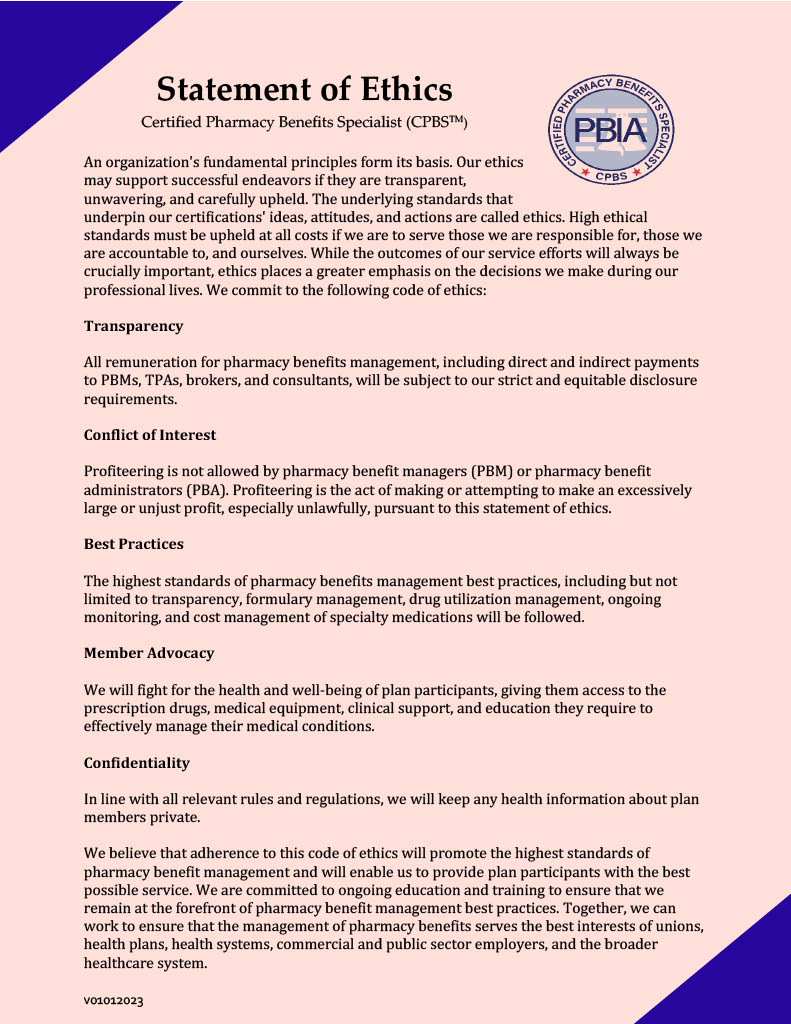
For Directors of Benefits and CFOs, understanding these four cost drivers and their components is critical not just for managing expenses, but also for improving patient outcomes without compromising care quality. By integrating strategic management of price, product mix, utilization, and cost sharing, organizations can achieve a more sustainable and efficient pharmacy benefit framework that upholds a fiduciary standard of care. This comprehensive approach ensures that costs are contained not by cutting corners, but by enhancing the value delivered to beneficiaries.