Turns out CVS’s “New” Guaranteed Net Cost Pricing Model is More of the Same – That is Bait and Switch
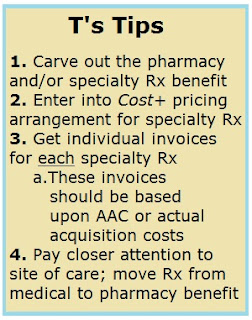 About a month ago I wrote, “Under the new model, CVS Health will return 100% of drug rebates to employer-sponsored groups and at some point in the future government health programs. The good news is this moves the entire industry one step closer to radical transparency.
About a month ago I wrote, “Under the new model, CVS Health will return 100% of drug rebates to employer-sponsored groups and at some point in the future government health programs. The good news is this moves the entire industry one step closer to radical transparency.The bad news is CVS Health admits it hoodwinked all those clients it sold pass-through arrangements. Those so-called pass-through agreements were nothing more than fee-for-service [opaque] pricing models disguised as pass-through contracts.
It’s safe to assume Caremark’s (CVS Health’s PBM) gross margins will grow next year or worst case remains flat. Shareholders wouldn’t have it any other way. So it begs the question, how?” Then I outlined a few ideas.
It didn’t take long for someone to present a serious challenge to CVS’s “new” guaranteed net cost pricing model. I’ve followed Dr. Abrams for several years and his research hits the mark. Turns out CVS’s new “Guaranteed Net Cost” model is more of the same that is bait and switch.