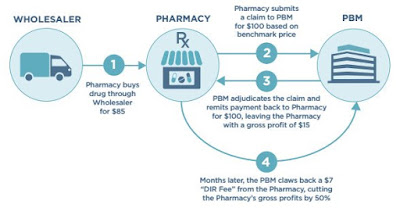
Understanding the Complexity of DIR Fees
 |
| Source: Diplomat Pharmacy |
DIR fees originated in Medicare Part D, however, these fees are now utilized for commercial plans. Pharmacies are charged DIR fees by PBMS after the point of sale. DIR fees may be based on pharmacy performance, ability to participate in a preferred network or as reconciliation between negotiated price and a claim.2 DIR fees have come under scrutiny by pharmacies. According to the White Paper: DIR Fees Simply Explained, DIR fees “create losses in revenue that, at times, may surpass the acquisition cost of the drug itself.” Moreover, certain pharmacy organizations have advocated for DIR fee reform. 3
1) DIR fees hide the true cost of the drug, from the plan sponsor, to the PBMs financial benefit. For example, PBMs might break-even on retail pharamcy network discounts on the front-end only to make up for it on the back-end through DIR fees. PBMs should be negotiating these discounts on behalf of the client then passing these savings onto plan sponsors. At the very least, PBMs should be disclosing their take home on these fees to plan sponsors.
2) Members cost share (i.e. coinsurance) too doesn’t take into account the PBM’s true cost when DIR fees are collected. If these fees were applied at the point-of-sale these plan participants would pay less and in some cases significantly so.
Alternately, make sure any contracting entity that might negotiate on your behalf (PSAO) explains to you the parameters of all of your contractual terms.”5








