Chelsea Handler ‘Didn’t Know’ She Was on Ozempic [Weekly Roundup]
Chelsea Handler ‘didn’t know’ she was on Ozempic and other notes from around the interweb:
- Health plan fiduciary breaches persist under CAA. The Consolidated Appropriations Act of 2021 (CAA) is the most significant compliance challenge employers have faced since the Affordable Care Act. Benefit advisers who serve the health and welfare side of our industry no doubt will need to continue paying close attention to this landmark legislation on behalf of their employer clients. New requirements are now in effect. They include the review of plan contracts and removal of all “gag clauses;” determination of “reasonableness” for vendor fees and services; prescription drug reporting for plan years 2020, 2021 and 2022; and analysis of parity between medical and mental health coverage. Failing to comply with these requirements leaves employers at risk of incurring fines and facing class-action lawsuits. But most organizations are still in the dark, believing their broker or TPA will handle compliance on their behalf, or that it’s simply “no big deal.”
- Chelsea Handler ‘Didn’t Know’ She Was on Ozempic, Says Her Doctor ‘Just Hands It Out to Anybody’. Chelsea Handler talked about Ozempic being used for weight loss in Hollywood circles — and shared her own experience — during her appearance on Call Her Daddy. The comedian, 47, sat down with host Alex Cooper for an intimate conversation on the podcast, where she opened up about unknowingly being prescribed Ozempic, intended to treat Type 2 diabetes. “So, my anti-aging doctor just hands it out to anybody,” Handler admitted. “I didn’t even know I was on it. She said, ‘If you ever want to drop five lbs., this is good.’ However, the medication is not intended for people who need to lose just 5 lbs. Ozempic, or its counterpart Wegovy for people with obesity, works in the brain, and shifts the person’s fat mass set point, Dr. Ania Jastreboff, M.D., PhD., and an obesity medicine physician scientist at Yale University told PEOPLE. Further, the drug needs to be taken at a low dose at the beginning, and slowly increased over time. Chandler says she gave herself a dose after a vacation. “I came back from a vacation, and I injected myself with it. I went to lunch with my girlfriend a few days later, and she was like, ‘I’m not really eating anything. I’m so nauseous, I’m on Ozempic,'” she recalled. “And I was like, ‘I’m kind of nauseous too.’ But I had just come back from Spain and was jet-lagged.” Handler then said her friend asked if she was sure she wasn’t on Ozempic before sharing that she was just “on semaglutide.” “That’s Ozempic,” her friend explained.
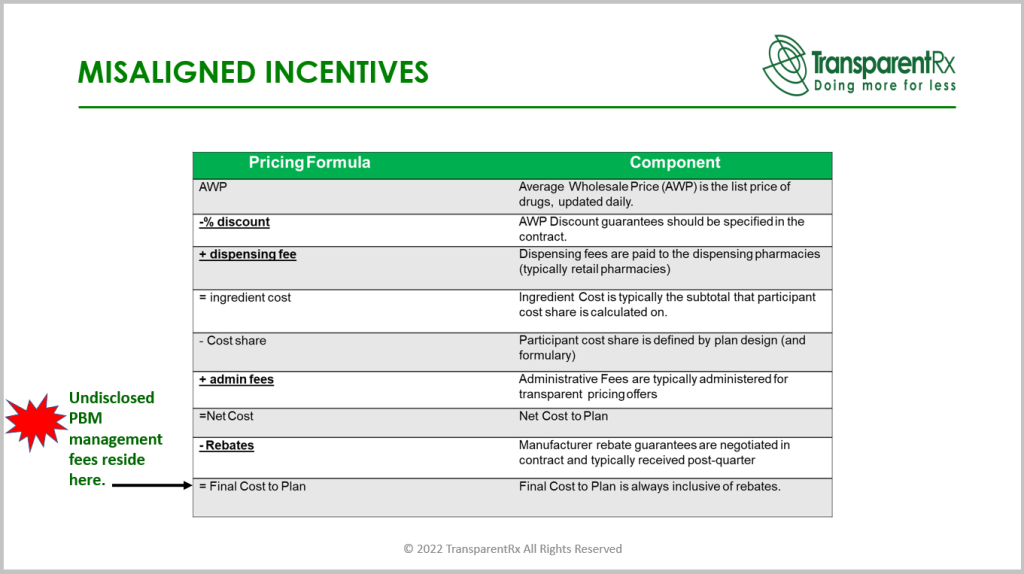
- Why Now Is the Time for Health Plans to Take Control of Pharmacy Benefits. It’s worth belaboring the point: PBMs are under the watchful eye of state and federal governments. The PBM of the future isn’t a gas-guzzling, polluting SUV, for example, it is an efficient, state-of-the-art, fully customizable electric vehicle. It is regulatory compliant and uses the best technology to ensure equitable pricing methodology, financial value, and great member experience. Instead of shrouding drug pricing in secrecy, new PBM business models rely on transparency. The best way to create an efficient and fair market is to allow both the buy and sell sides of the transaction to communicate freely about how drug prices are set, rebates, and other essential information. On the compliance side, plan sponsors must recognize and understand how their health plan drives revenue for their benefits brokers and consultants (e.g., are they compensated for recommendations on pharmacy benefits or any other aspect of health benefits?). The Consolidated Appropriations Act of 2021 places new fiduciary responsibilities on entities that provide health benefits, and plan sponsors must ask their broker or consultant to disclose how they’re compensated.
- Summit County sues pharmacy benefits managers over opioid crisis. Governments, insurers, or employers typically hire pharmacy benefit managers to facilitate prescription drug programs, with the goal of reducing costs for the insured. The lawsuit, however, accuses the companies of doing the opposite. It alleges the businesses colluded with manufacturers to make opioids more available for pain treatment and by ignoring clear warning signs of addiction in patients. The companies did so to increase profits, the lawsuit said. “Whether by colluding with manufacturers to make opioids more available as a form of pain treatment or by ignoring the mounting evidence of addiction and misuse in their own claims data, [pharmacy benefits managers’] role in creating and sustaining the opioid epidemic is largely hidden from public scrutiny but nevertheless facilitated the reckless promotion of opioids by manufacturers, the oversupply of opioid shipments by distributors and the irresponsible dispensing of prescription opioids by numerous pharmacies,” the lawsuit said.