In 2019, Dean Foods, which this year was acquired by Dairy Farmers of America, spent $52,900 on 4 biosimilars, well short of the $227,500 the company would have spent on 3 originator products. The carve-out was arranged through Vivio and enabled Dean Foods to sequester specialty drug costs and management so that savings could be achieved outside of the structure imposed by a pharmacy benefit manager (PBM) plan.
Switching employees on expensive originators to biosimilars, generic drugs, and lower-cost therapeutic alternatives while also discontinuing experimental drugs generated $1.7 million in clinical savings (avoided therapy costs) for the former dairy company, the report said. But given all anticipated vs actual costs from the carve-out program, Dean Foods saved $4.35 million in 2019, according to the report. This includes supply chain savings.
Tyrone’s Commentary:
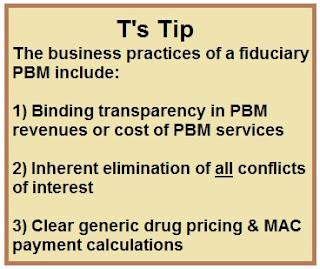
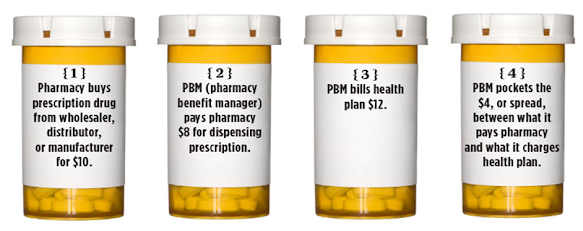
There are several benefits to a carve-out PBM arrangement including options to carve out specialty pharmacy. The truth is if left to their own devices specialty pharmacies owned by PBMs, or independent, want to get the product out of the door and into the mail. When left unchecked, there is little chance it will pass up on filling a $15,000 prescription knowing full well a less costly therapeutic alternative is as effective. It is up to the plan sponsor to remove any conflict of interest.
Benefits of a carve-in PBM arrangement such as population health management can make life easier. When all the data is under one roof it goes without saying life is easier compared to bringing in a third-party. However, plan sponsors have to be careful though what you give up in exchange for “easier.” With carve-in arrangements plan sponsors can lose flexibilty and control of benefit design, formulary management and even forgo rebate dollars. Of course, no carved-in PBM will tell you this is going to happen just read between the lines.
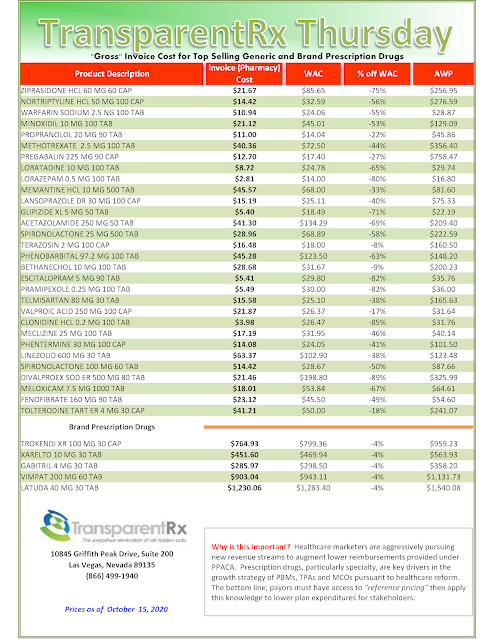
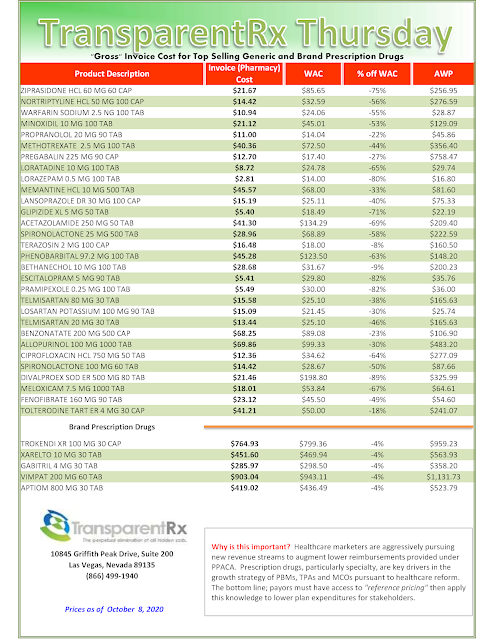
Vivio said in the report it achieves savings by seeking out lowest-cost drug suppliers, passing 100% of rebates to its customers, and taking advantage of manufacturer discounts. It said that “typically, 15% of prescribed specialty drugs have lower-cost therapeutic equivalents alternatives such as biosimilars, generics, and less-costly branded drugs.”
Continue Reading >>