Tuesday Tip of the Week: 3 Ways Savings Could be Achieved by Improving Pharmacy Benefit Design and Management
PBMs or pharmacy benefit managers have large scale, highly automated operations to process claims and provide customer (client and member) service. The services a PBM provides can be categorized as administrative or clinical. Administrative services include benefit administration, enrollment and eligibility administration, pharmacy network administration, mail pharmacy service, claims adjudication, and manufacturer contracting and rebate administration. Clinical services range from formulary management to sophisticated utilization and disease management programs.
PBM services revolve around the drug benefit designed by the client. The benefit design determines the drugs that are covered, and the extent to which generics and formulary drugs are mandated. As a part of the drug benefit, a co-pay structure is developed which determines the cost sharing between the client and its employees or members. PBMs receive enrollment information from their clients and maintain the pharmacy benefit eligibility files.
Plan sponsors could lower drug spending and out-of-pocket costs for enrollees by reducing the use of high-cost, low-value drugs on formularies. PBMs provide a range of services including formulary development, clinical care management, utilization management (including preauthorization), negotiations with pharmacies for drug price discounts, negotiations with manufacturers for rebates, and claims adjudication and payment.
Plan sponsors use services depending on their individual models and preferences; administrative fees are assessed accordingly. Services with the potential to increase revenue streams to the PBM may lower administrative fees; for example, formulary design that allows PBMs to select “profitable” drugs in terms of rebates and pharmacy spread might be accompanied by reduced administrative fees. Plan sponsors have made unfavorable and often uninformed trade-offs for reduced administrative fees to PBMs. Here are three ways savings could be achieved by improving pharmacy benefit design and management.
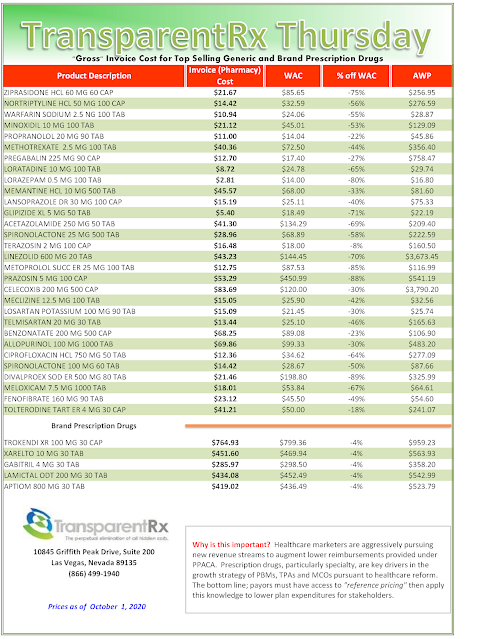
1) Eliminate wasteful or low-value drugs which includes me-too drugs (immaterial tweaking of a particular ingredient results in a “new” drug that adds no clinical value and often extends patent protection), combination drugs or drugs that combine two active ingredients into one pill resulting in costs substantially higher than the costs of the individual ingredients, prescription drugs offered when over-the-counter alternatives are available, and brand-name or higher-priced generic drugs offered when lesser-cost generics are available
2) Compare reduced per-member per-month drug spend that can result from an appropriate drug mix instead of the current conventional procurement processes involving consultants comparing administrative fees, rebates, and discounts.
3) Make the PBM’s management fee the #1 metric when evaluating PBM proposals and performance. The revenue a PBM keeps for itself is referred to as its management fee. In other words, it is the fee a PBM charges a client for the services it was hired to perform. PBM management fees are a hidden driver of pharmacy costs. While discount guarantees, rebates and clinical management are very important, they are also being used to distract purchasers from a key driver of their final plan costs – PBM management fees.