The Next BIG Thing in Prescription Drugs is in Your Pocket!


 |
| Compliance Packaging: Integral part of any good MTM program |
_1.jpg) | |
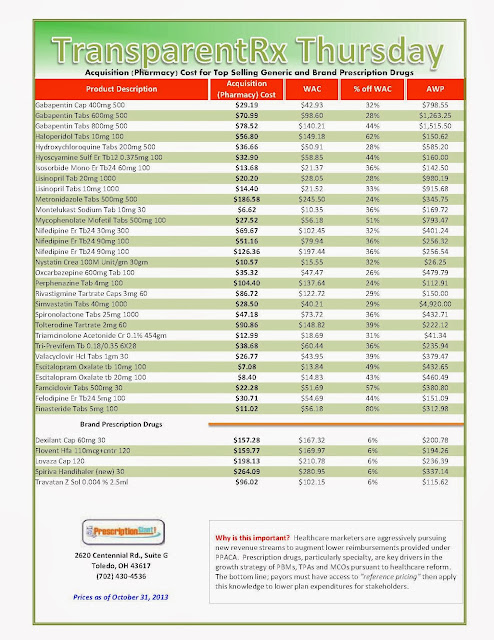
As of 10/31/2013 – Published Weekly on Thursdays
Step #1: Obtain a price list for generic prescription drugs from your broker, TPA, ASO or PBM every month. Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list. Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions. Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our pharmacy cost then determine if a problem exists. When there is a 10% or more price differential (paid versus actual cost) we consider this a problem. Multiple price differential discoveries means that your organization or client is likely overpaying. REPEAT these steps once per month. Include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to see if better pricing is available in the marketplace compared to what the client is currently receiving. When better pricing is discovered the contract language should stipulate the client be indemnified. Do not allow the PBM to limit the market check language to a similar size client, benefit design and/or drug utilization. In this case, the market check language is effectually meaningless. |
I welcome any comments you may like to post. In addition, feel free to contact me at tyrone_squires@transparentrx.com or call (702) 430-4536.
_1.jpg) |
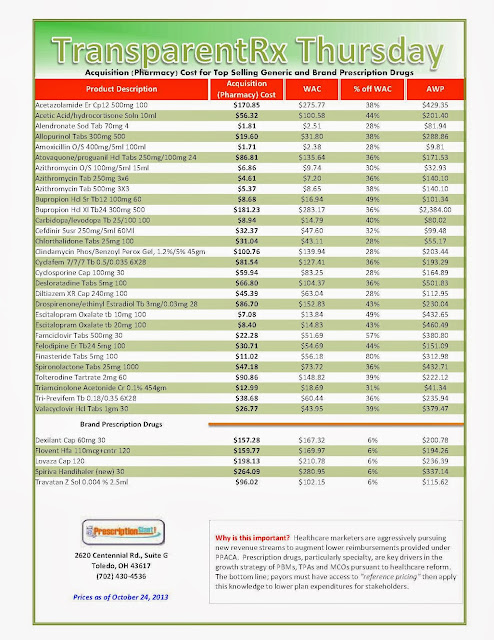
| As of 10/24/2013 – Published Weekly on Thursdays |
| How to Determine if Your Company [or Client] is Overpaying |
An editorial in today’s JAMA decries the price of the orphan drug Ivacaftor (Kalydeco), a product of Vertex Pharmaceuticals for cystic fibrosis patients who carry a specific mutation. The price is $311,000 – although some patients could pay as much as $373,000. The drug would be taken for decades.
_1.jpg) |
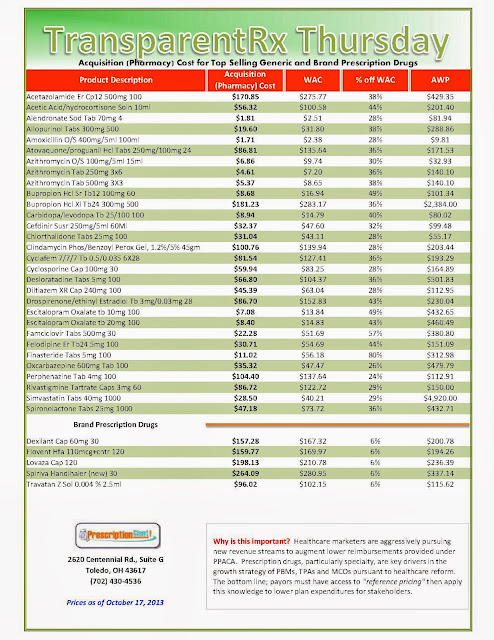
| As of 10/17/2013 – Published Weekly on Thursdays How to Determine if Your Company [or Client] is Overpaying |
While the aforementioned tactics do assist in controlling costs, they’re standard practice and are not the aggressive measures necessary to help reduce or control spending. An excellent PBM is one which truly puts its clients and their members first; before shareholders and profitability. Hire the right PBM, one willing to follow through on these 7 steps, and you’ll surely rein in rising drug costs.
_1.jpg) |
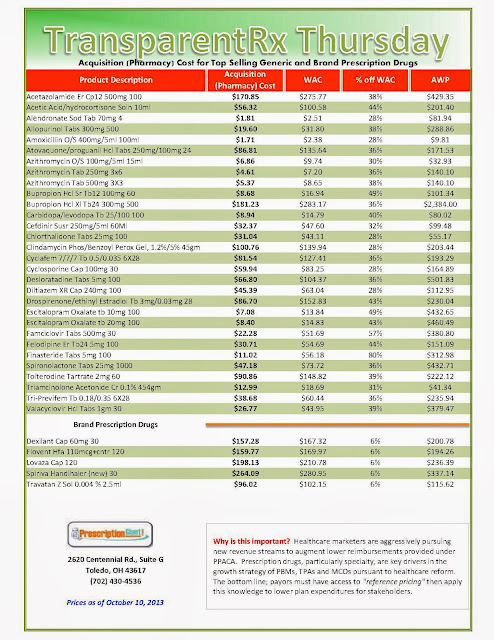
| As of 10/10/2013 – Published Weekly on Thursdays |
Step #1: Obtain a price list for generic prescription drugs from your broker, TPA, ASO or PBM every month.
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our pharmacy cost then determine if a problem exists. When there is a 10% or more price differential (paid versus actual cost) we consider this a problem.
Include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to see if better pricing is available in the marketplace compared to what the client is currently receiving.
When better pricing is discovered the contract language should stipulate the client be indemnified. Do not allow the PBM to limit the market check language to a similar size client, benefit design and/or drug utilization. In this case, the market check language is effectually meaningless.
And while private exchanges have been gaining traction in the last couple of years, the role of pharmacy still appears to be evolving, with some PBMs pursuing carve-out options and others seeking to operate as partners to the health plan participants. A private exchange allows employers to offer more benefit design choices to employees and in some cases set a defined contribution toward coverage. If workers select a more expensive health plan, they pay the difference in premiums. Some private exchanges make available benefit designs from several different insurers. Other private exchanges are operated by a single carrier and only stock that carrier’s plans. Depending on the exchange model, the health plans may be fully insured or self-funded.

Reprinted from DRUG BENEFIT NEWS, biweekly news and proven cost management strategies for health plans, PBMs, pharma companies and employers.