One of the first questions I often get during a new consulting assignment centers around cost data. More specifically, analyzing the cost of one proposal against that of another PBM vendor. When this happens I know there could be some trouble ahead for our partnership.
Where costs are concerned, I’m most concerned with whether or not rebates, discount rates and dispensing fees are competitive. It takes all of 30 minutes to compare these data points among 5 to 7 competing PBM vendors. Once I know pricing is competitive my attention turns to the contract.
You see PBMs don’t set prices they negotiate for better pricing which is different than setting prices. All bets are off if the PBM repackages directly via a mail-order pharmacy or indirectly through say a national chain of retail pharmacies. More about this later.
During Bill Clinton’s 1992 successful presidential campaign, James Carville coined the phrase “It’s the economy, stupid!” For our purposes and stealing a page from James Carville, “It’s the contract, stupid!” All kidding aside, the contract will determine what you ultimately pay so in a sense words matter more than numbers.
Here are seven PBM contract pitfalls you should not ignore.
1. Begin procurement at least six months before the renewal date to put your company in the best position to drive a hard bargain. The first day of procurement starts when you’ve sent the RFI notification letter not when you’re just talking about renewal. Don’t wait too long before you begin procurement. Incumbent PBMs and other stakeholders love it when the process is rushed. The reasons should be obvious.
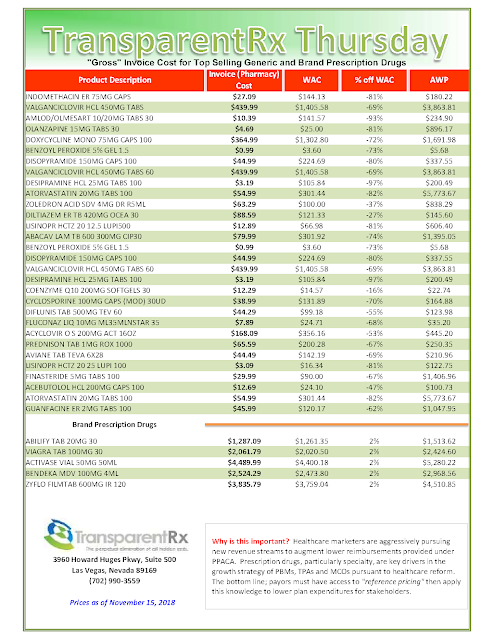
2. Presuming you have strong contract definitions, make sure rates and fees are in alignment with those definitions. The problem is 75% of buyers, from Fortune 500 companies to start-up, have bad language in their contracts. Just below is an example of bad contract language. Can you spot the problem areas? If you’re a decision-maker and you can’t, get some training or hire someone to help with managing your pharmacy benefit, seriously.
 |
| Click to Enlarge |
3. Don’t allow the PBM to use an in-house definition for rebates, brand, generic or specialty drugs. The devil is in the details and non-fiduciary PBMs rely on wordplay to access hidden revenue streams.
4. During a RFP process, never select a winning vendor before contract terms have been agreed to by both parties. Believe it or not more than 50% of buyers make this mistake and it costs them radical transparency.
5. Always include market check language in your contract.
6. Don’t permit the PBM to put a ceiling on penalties for failing to meet performance guarantees. One exception to the ceiling rule is when the financial penalty exceeds the amount of fees paid. Put 50-100% of PBM fees at risk, up to the amount of fees paid, when guarantees aren’t met.
7. Your general counsel and CFO are likely unqualified to uncover hidden PBM cash flows even less so to measure the impact of clinical services. Get training or hire a PBM expert who has extensive experience in PBM contract review and a track record of success. This will save thousands of dollars and depending on the size of your company maybe even millions of dollars. Check out what Michael Critelli, now retired CEO of Pitney Bowes, wrote to me a couple years back.
 |
| Click to Enlarge |
Weighting the importance of each (cost analysis vs. contract language) in terms of what an employer might pay, contract language is 90% and cost analysis is 10%. Non-fiduciary PBMs don’t set prices instead they manipulate prices which have been established by manufacturers, or wholesalers.
Worse yet, non-fiduciary PBMs negotiate fearlessly with manufacturers primarily to fill their own coffers. Saving clients money is an ancillary benefit and not the priority despite the rhetoric coming out of these shops. If you don’t believe me and think I’m hating just follow their earnings calls.
Think about it…the key then to bending the prescription drug cost trend is to reduce the amount of cash non-fiduciary PBMs keep for themselves which is based largely on your utilization. The key to uncovering these hidden cash flows is the contract language. A word to the wise, don’t put too much emphasis on spreadsheet analysis.