Largest pharmacy benefits manager in the U.S. accused of costing the New York City Transit Authority tens of millions of dollars
New York City Transit staff first noticed a spike in claims for pricey compounded medications as claims surged from less than $500,000 a month in 2015 to $8.8 million in March 2017. In June 2016, Transit officials noticed one of those claims was $405,326 for three months of compounded medication for erectile dysfunction, according to the lawsuit.
“The $400,000 erectile dysfunction claim proved non-fraudulent,” the suit notes. “Yet, compound medication costs continued to rise for suspicious reasons that should have provoked an aggressive response from ESI.”
Tyrone’s Commentary:
 |
| Click to Learn More |
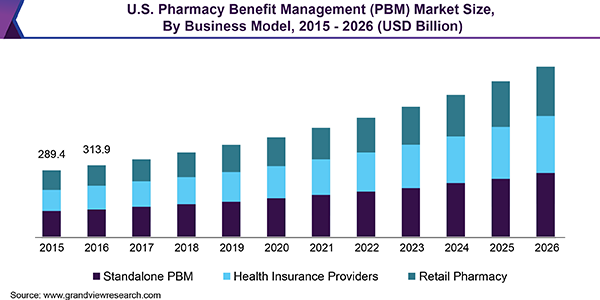
Non-fiduciary PBMs generate most of their profit from three sources:
1) Spread Pricing
2) Rebate Spreads
3) Benefit Design
If a plan sponsor closes or limits #1 and #2 during contract negotiations, a non-fiduciary PBM will shift that lost revenue to #3. The NYC Transit Authority didn’t realize this fact until it was too late. That $400,000 claim, much of it went to ESI. Even worse, the NYC Transit Authority had to sign off on the plan design allowing these claims to get adjudicated.
You are probably thinking this couldn’t happen to me and you would be wrong. It is happening you just don’t know how to uncover it or have turned a blind eye. Continuous Monitoring or CM would have identified this problem before it got out of hand. Audits occur 12 months after the fact which is too late to claw back overpayments. Continuous Monitoring on the other hand, catches and resolves overpayments or other issues much much faster.
A word to the wise, stop using claims re-pricings as the holy grail for evaluating a PBM’s service cost. Just as important, if not more so, is how well a PBM manages product mix and utilization. If a PBM manages product mix poorly, you are asking another PBM to compare prices for those same poorly managed Rx’s.
There is potentially significant savings between a pharmacy plan that is managed efficiently compared to one that is inefficient. That can’t be uncovered in a claims dump alone. Ignore this and you will overpay just like the NYC Transit Authority.
According to the lawsuit, NYCTA paid $20 million in 2016 for compounded medication prescribed by a single California orthopedic surgeon who, in the previous year, was snared in a workers’ compensation kickback scheme. And in 2017, the suit says, one Utah pharmacy was responsible for $20 million of New York City Transit’s compounded medication tab.
Continue Reading >>