PBMs with a traditional business model typically allow for price spread in exchange for reduced or eliminated administrative fees. It can generate a significant percentage of its revenue by retaining the spread from the MAC list. In some cases, this may be disclosed; however, plan sponsors are often not aware of how much revenue the traditional PBM retains. Auditing of this process is often very difficult.
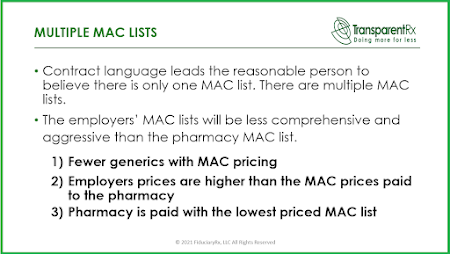
With this method, the traditional model PBM uses an aggressive MAC price list to buy from their contracted pharmacies and a different, less aggressive list of prices when they sell to their clients. In essence, these PBMs buy low, and they sell high with their MAC price lists, marking up what they buy. The money derived from using multiple MAC lists goes into the pocket of the traditional PBM.
In contrast, a PBM with a radically transparent, pass-through business model does not keep the spread. Instead, this type of PBM uses one MAC list for all purposes: buying from the pharmacies and selling to the client, and then passing through the same drug cost, without markup, to the client. All discounts accrue directly to the benefit of the client (and member).
MAC prices are the upper limits that a plan will pay for generic drugs and brand drugs that have generic versions available (multi-source brands). Generic drugs often have a huge range of Average Wholesale Prices (AWPs), and the MAC prices are needed to reconcile the differences between an inflated AWP and the price the pharmacy actually pays.
No two MAC price lists are alike. In other words, every PBM tends to pick and choose products for their MAC lists, using different criteria to derive and apply prices to the lists. Common criteria for inclusion of products on MAC lists include:
- It’s a balancing act. The PBM’s goal is to work on behalf of its clients and members, bringing the best value, without unduly creating unrest among pharmacies.
- There are basically two ways the PBM can handle the MAC price list: 1) they can be self-serving and operate a MAC list to generate revenue for themselves or, 2) they can fully pass-through all MAC discounts directly to the client.
A radically transparent, pass-through PBM’s only revenue source is an administrative fee that is typically calculated on a per paid claim or per-member, per-month (PMPM) basis. Any gains in pricing negotiated with pharmacy networks or pharmaceutical manufacturers are passed directly on to the client, at the beginning and throughout the course of the contract.
Be careful, PBMs can be transparent and still keep a spread using their MAC lists. Generally, pass-through pricing means that the PBM passes the discounts, rebates, other revenues and actual costs charged by the pharmacy or paid by a pharmaceutical company (in the form of rebates) directly on to the plan sponsor. In actual use, it can have various definitions according to the understanding of the parties.
The term “pass-through” must be carefully defined in the contract in every instance it is used since there is no industry standardized term. A PBM may tell you that it will be transparent and pass-through, however, when presented with strict terms, the PBM may not be willing to abide by those terms. In summary, “transparent” PBMs are not necessarily “transparent pass-through” PBMs. While it may seem like a trivial distinction, it really isn’t.
 “Thank you Tyrone. Nice job, good information.” David Stoots, AVP
“Thank you Tyrone. Nice job, good information.” David Stoots, AVP