An article was just published by Jonathan Swichar a trial attorney who specializes in pharmacy litigation. The title of the article is “PBMs Keep ERISA Preemption Fight Alive.” The screenshot is from a questionnaire TransparentRx submits in response to RFPs.
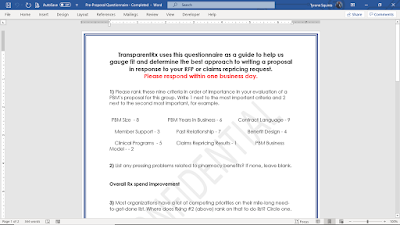 |
| Click to Enlarge |
Ninety percent (90%) of the responses we receive rank claims repricing the #1 factor in evaluating PBM proposals. Can we for goodness sakes put an end to this practice? Claims repricings should not be your most important tool in evaluating PBM proposals.
There is parity in network pricing across the PBM industry. No one PBM has a decided advantage over another no matter their size or the price benchmark being used whether it is AWP minus, MAC, NADAC etc.
The key then is what happens after the plan goes live? When your ingredient costs exceed that of the PBMs (pharmacy reimbursement) does the PBM return the overages to you or keep it for themselves, for example? You rely on claims repricings because 1 +1 = 2 and downplay the importance of contract nomenclature. Big mistake.
Non-fiduciary PBMs print money by leveraging this sort of unsophistication to their financial advantage. It’s no surprise PBMs who don’t volunteer radical transparency are attempting to circumvent SCOTUS’s ruling.