 |
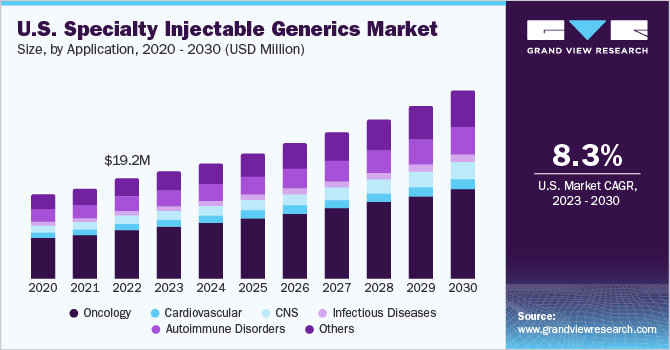
| Source: Grandview Research |
Non-fiduciary PBMs are generally left alone to define what constitutes a specialty drug. I write “generally” because PBMs will rely on the demands of clients for how much disclosure (i.e. transparency) they will provide. When left to their own accord, non-fiduciary PBMs will classify drugs as specialty which shouldn’t be specialty by any reasonable measure including the MediSpan Master Drug Database or MDDB.
Secondly, these PBMs will steer patients to their “specialty pharmacies” by offering what appear to be better discounts or rebates to unwitting plan sponsors. In this case, the non-fiduciary PBMs, which own specialty pharmacies, are sending money that self-funded employers and their subscribers are paying for the specialty drugs right back into the PBMs’ own bank account. The PBM still meets its discount guarantee but that doesn’t tell the entire story. You must know what the pharmacy is being reimbursed! Without that information well…see Senator Dave Burke’s analogy below.
The report “Medicine Use and Spending in the US,” found that overall medication spending increased by 0.6% in 2017 after off-invoice discounts and rebates, including spending on all types of medications. The report notes that specialty medications are rapidly approaching half of overall medicine spending, while net spending on retail and mail-order pharmacy distribution dropped 2.1% in 2017.
Invest more time and money into becoming a better steward of pharmacy benefits. Incrementalism in this area will not be rewarded. The best proponent of radical transparency are educated purchasers of PBM services. Senator Dave Burke explains it best, “If you knew how much a yard of concrete costs, you know how many yards are in a mile and you can estimate how much you should spend on concrete…When the person who is doing that work isn’t telling you how much they paid for the concrete – they just tell you how much it costs for a mile of road – that gets to be a very expensive highway.”
