Just because a drug is approved by the FDA, does not mean it has proof of efficacy [Weekly Roundup]
News and notes from around the interweb:
- Just because a drug is approved by the FDA, does not mean it has proof of efficacy. Medicare spent nearly $600 million over a three-year period to pay for cancer care involving four drugs later found to provide no clinical benefit for some forms of the disease for which the Food and Drug Administration approved them, an analysis published Monday, October 18, 2021 by JAMA Internal Medicine found.
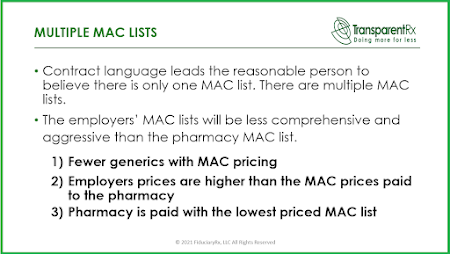
- An attorney shares the warning signs of ‘self-serving’ PBMs. PBMs are designed to manage prescription drug benefits on the behalf of health insurers, saving both insurers and consumers money on prescription drugs. However, as the pharmaceutical industry has ballooned and drug prices have increased 33% since 2014, questions have been raised over whether PBMs are acting in the interest of their clients.
-

Join the Movement! Large Private Employer Coalition Creates Pharmacy Benefit Management Firm. A nonprofit coalition of nearly 40 private employers, including U.S. retailers Walmart and Costco, has launched a new company that would offer pharmacy benefit management (PBM) services for employers.
- How PBM “rebate walls” impact drug spending, patient care and competition. Federal agencies and plan sponsors—the clients of PBMs—are beginning to explore perverse PBM incentives and are waking up to abusive PBM practices.
- Strategies for Aligning and Integrating Infusion Services Across the Health System. Nancy Palamara, PharmD, the vice president for diagnostics and therapeutics at Holy Name Medical Center, in Teaneck, N.J., polled session attendees as to who at their institution has operational oversight of the outpatient infusion center and all of its staff. The most common response was a nurse manager (35%), followed by a nonclinical manager (15%), pharmacist (4%) and physician (2%); 31% of respondents said oversight was handled by a mix of those roles, while 13% did not know.