What might the Amazon, Berkshire and JP Morgan health care joint venture actually do?
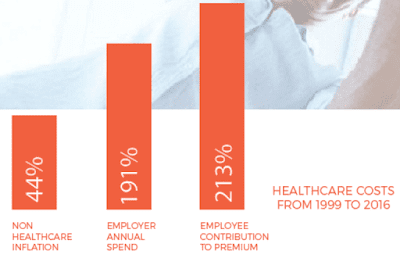 |
| Source: Health Transformation Alliance |
A report on CNBC indicates that JP Morgan would like the effort to reduce the $1.5 billion they spend on employee health care by 20%. What will ABJ actually do and will they be successful?
Before answering the previous question, it is essential to understand both the nature and magnitude of the health care problems that exist today in the United States. Warren Buffett frames the core problem with US health care system succinctly: “In almost every field of American business, it pays to bring down costs. There’s … no incentive to bring down costs.”
Charlie Munger has described many times how perverse incentives can create a horrific result: “If the incentives are wrong, the behavior will be wrong. I guarantee it. Not by everybody, but by enough of a percentage that you won’t like the system.” “Show me the incentive and I will show you the outcome.” “I think I’ve been in the top 5% of my age cohort all my life in understanding the power of incentives, and all my life I’ve underestimated it. Never a year passes that I don’t get some surprise that pushes my limit a little farther.”








