“Don’t Miss” Webinar: How to Slash PBM Service Costs, up to 50%, Without Changing Vendors or Benefit Levels
Here is what some participants have said about the webinar.
“…Great presentation! I had our two partners on the presentation as well. Very informative.” Nolan Waterfall, Agent/Benefits Specialist
A snapshot of what you will learn during this 30 minute webinar:
- Hidden cash flows in the PBM Industry such as formulary steering, rebate masking and differential pricing
- How to calculate cost of pharmacy benefit manager services or CPBMS
- Specialty pharmacy cost-containment strategies
- The financial impact of actual acquisition cost (AAC) vs. effective acquisition cost (EAC)
- Why mail-order and preferred pharmacy networks may not be the great deal you were sold
Tyrone D. Squires, MBA
TransparentRx
2850 W Horizon Ridge Pkwy., Suite 200
Henderson, NV 89052
866-499-1940 Ext. 201
P.S. Yes, it’s recorded. I know you’re busy … so register now and we’ll send you the link to the session recording as soon as it’s ready.
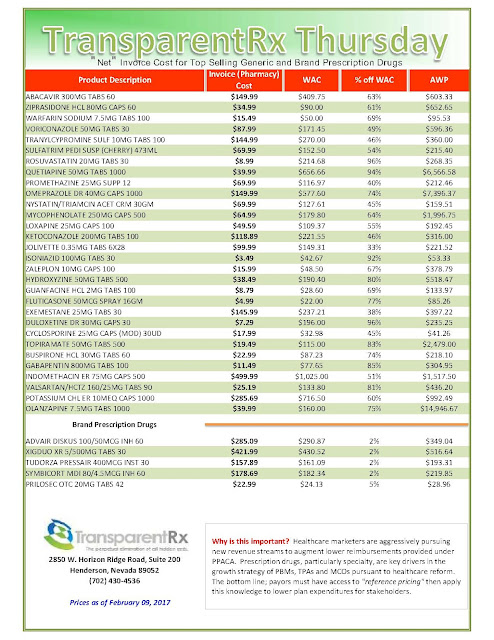
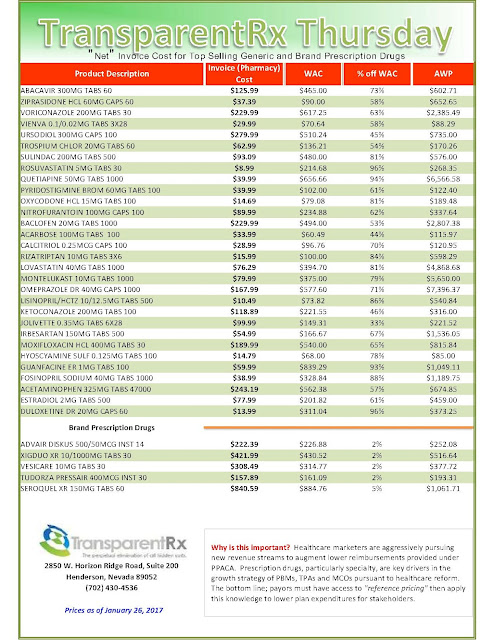
“Gross” Invoice Cost for Top Selling Generic and Brand Prescription Drugs – Volume 154
The costs shared here are what the pharmacy actually pays; not AWP, MAC or WAC. The bottom line; payers must have access to actual acquisition costs or AAC. Apply this knowledge to hold PBMs accountable and lower plan expenditures for stakeholders.
Step #1: Obtain a price list for generic prescription drugs from your broker, TPA, ASO or PBM every month.
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our acquisition costs then determine if a problem exists. When there is a 5% or more price differential (paid versus actual cost) we consider this a problem.
Multiple price differential discoveries means that your organization or client is likely overpaying. REPEAT these steps once per month.
— Tip —
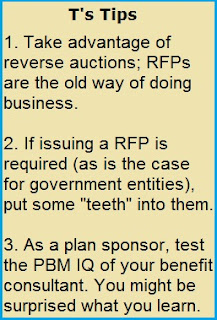
Always include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to determine if better pricing is available in the marketplace compared to what the client is currently receiving.
When better pricing is discovered the contract language should stipulate the client be indemnified. Do not allow the PBM to limit the market check language to a similar size client, benefit design and/or drug utilization. In this case, the market check language is effectually meaningless.
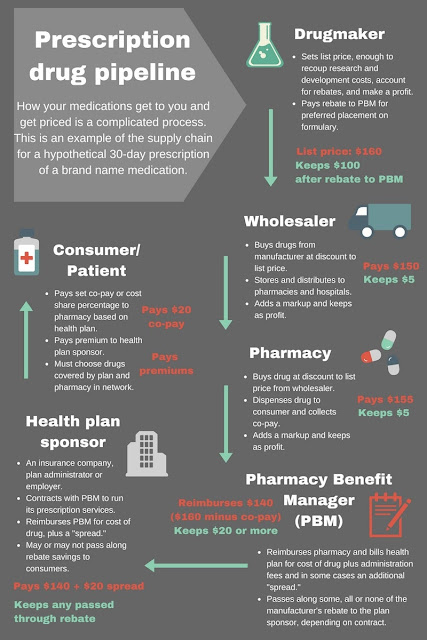
Six Takeaways: How are prescription drug prices set?
 |
| Click to Enlarge |
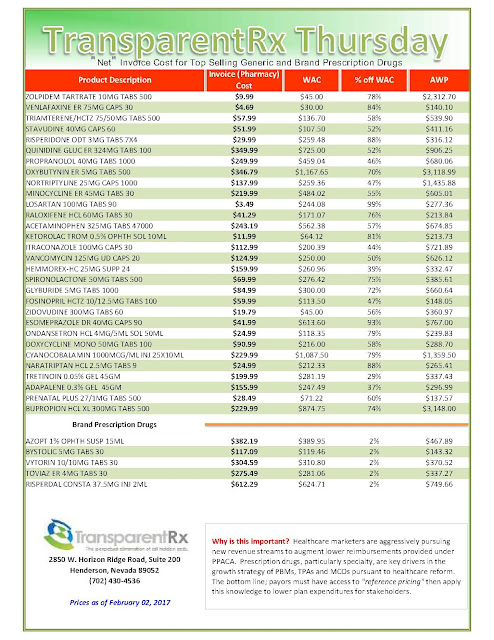
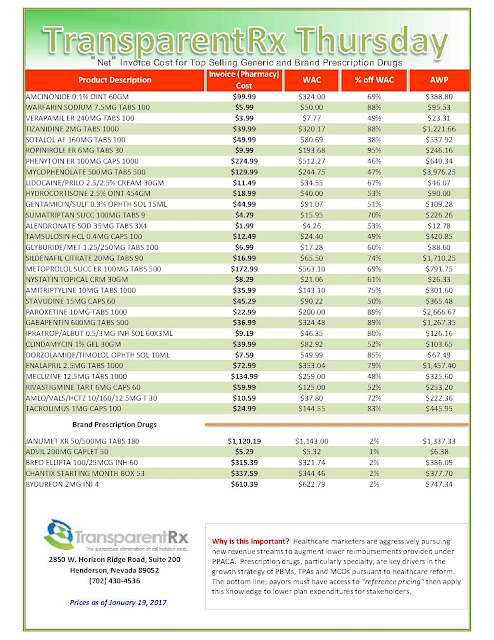
“Gross” Invoice Cost for Top Selling Generic and Brand Prescription Drugs – Volume 153
The costs shared here are what the pharmacy actually pays; not AWP, MAC or WAC. The bottom line; payers must have access to actual acquisition costs or AAC. Apply this knowledge to hold PBMs accountable and lower plan expenditures for stakeholders.
Step #1: Obtain a price list for generic prescription drugs from your broker, TPA, ASO or PBM every month.
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our acquisition costs then determine if a problem exists. When there is a 5% or more price differential (paid versus actual cost) we consider this a problem.
Multiple price differential discoveries means that your organization or client is likely overpaying. REPEAT these steps once per month.
— Tip —
Always include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to determine if better pricing is available in the marketplace compared to what the client is currently receiving.
When better pricing is discovered the contract language should stipulate the client be indemnified. Do not allow the PBM to limit the market check language to a similar size client, benefit design and/or drug utilization. In this case, the market check language is effectually meaningless.
Pharmaceutical Companies Not Seeing Majority of Drug Revenue
In a study conducted by Berkeley Research Group, the investigators found that pharmaceutical companies only realize 39% of initial gross drug expenditures.
Prescription drug spending has skyrocketed in the last few years, which has caused many stakeholders to demand increased pricing transparency. Pricing scandals, such as the recent outrage over EpiPen, has caused Americans to become skeptical about the reasoning behind dramatic drug price increases.
Certain measurements of drug costs do not show the whole picture, and can lead to an inaccurate picture of the gross spend by the customer, and an overstatement of the profits made by manufacturers, according to the study.
Although the chain of payment can be complicated, it can be summed up by 3 transactions: initial gross spending on the drugs by patients and insurers, discounts, and rebates/fees paid by the manufacturer. This multi-step chain of wholesalers, pharmacies, and other entities can create confusion about drug costs.
Wholesalers purchase the drugs that are then sold to pharmacies and healthcare providers, and pharmacy benefit managers (PBMs) negotiate lower prices through their buying power for certain health plans or employers.
Due to the lengthy supply chain, prices inflate down the line, which leads to patients paying higher prices for their prescription drugs. However, manufacturers do provide rebates and discounts to certain patients, health plans, or PBMs, which results in lower costs.
Additionally, manufacturers are required to provide significant discounts to government health plans and other government institutions, such as Medicare or Medicaid. This acts to reduce net spending by the government, but also reduces profits realized by pharmaceutical companies, according to the study.
In the study, the investigators considered rebates, discounts, and fees paid, to show a more complex picture of pharmaceutical manufacturers’ profits and spending.
“Gross” Invoice Cost for Top Selling Generic and Brand Prescription Drugs – Volume 152
The costs shared here are what the pharmacy actually pays; not AWP, MAC or WAC. The bottom line; payers must have access to actual acquisition costs or AAC. Apply this knowledge to hold PBMs accountable and lower plan expenditures for stakeholders.
How to Determine if Your Company [or Client] is Overpaying
Step #1: Obtain a price list for generic prescription drugs from your broker, TPA, ASO or PBM every month.
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our acquisition costs then determine if a problem exists. When there is a 5% or more price differential (paid versus actual cost) we consider this a problem.
Multiple price differential discoveries means that your organization or client is likely overpaying. REPEAT these steps once per month.
— Tip —
Always include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to determine if better pricing is available in the marketplace compared to what the client is currently receiving.
When better pricing is discovered the contract language should stipulate the client be indemnified. Do not allow the PBM to limit the market check language to a similar size client, benefit design and/or drug utilization. In this case, the market check language is effectually meaningless.
Diplomat Pharmacy, Inc. has published a new report on the state of specialty pharmaceuticals
 |
| Click to Enlarge |
The report offers insight on developments in emerging specialty therapies. Last year, the FDA Center for Drug Evaluation and Research (CDER) approved 22 novel new drugs. While there was a reduction in novel new drugs compared to previous years, there were several expanded indications for previously approved therapies that allowed these drugs to reach additional patient populations. New approvals included a mix of oncology, immunology, rare diseases, and other disease states.
Although the quantity of novel new drugs was lower in 2016, important new drugs became available in each of the broad disease states covered by specialty pharmacy. Specialty drug products accounted for approximately half of new drugs and biologics approved in 2016, similarly to in 2015. Nine specialty agents were approved for rare diseases.
“The specialty pharmacy industry continues to show exceptional growth,” said Paul Urick, Diplomat’s president. “The development of new drugs, as well as expanded indications for previously approved treatments continues to make the robust specialty drug pipeline one of the major drivers of growth.”
The pipeline is expected to produce more novel new oral oncology drug approvals in 2017 than in 2016, with multiple approvals forecasted in breast cancer and blood cancers.
To view the report, visit http://bit.ly/2jnTRwl.
Secret rebates erode drugmaker revenue, industry study says
 Of the estimated $349.1 billion that insurers and patients paid for brand-name drugs in 2015, $218.6 billion, or 63 percent, was realized as revenue by drugmakers, according to an analysis paid for by the Washington drug lobby, Pharmaceutical Research and Manufacturers of America. In 2013, pharma companies kept $177.5 billion, or 67 percent, of the $264.9 billion in gross expenditures for brand-name drugs.
Of the estimated $349.1 billion that insurers and patients paid for brand-name drugs in 2015, $218.6 billion, or 63 percent, was realized as revenue by drugmakers, according to an analysis paid for by the Washington drug lobby, Pharmaceutical Research and Manufacturers of America. In 2013, pharma companies kept $177.5 billion, or 67 percent, of the $264.9 billion in gross expenditures for brand-name drugs.
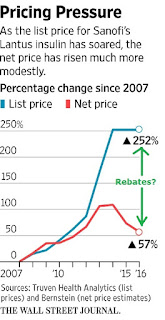
Pharmaceutical companies are facing pressure from Washington lawmakers and patients over increasing prices for medications such as insulin, which diabetics need to survive. At a press conference last week, President-elect Donald Trump said the industry is “getting away with murder” and threatened to force companies to bid for government business. Drugmakers say significant discounts and rebates paid to middlemen, such as pharmacy benefit managers that negotiate prices for insurers and other payers, reduce their revenue.
“Manufacturers are offering greater and greater rebates to gain access to patients,” Aaron Vandervelde, managing director at the Berkeley Research Group consulting firm and the report’s lead author, said in an interview. “That is largely offsetting the list price increases.”
Overall, branded drug makers paid $106.4 billion in discounts, fees and rebates to health plans, pharmacy benefit managers and U.S. government health programs in 2015, up from $67 billion in 2013, according to the report. The Berkeley analysis is one of the first attempts to add up the variety of rebates and discounts paid on brand-name drugs, exact details of which are closely guarded trade secrets.
The consulting group also estimated markups and fees taken at various stages of the drug supply chain, including by distributors, pharmacies and the health-care providers who administer medications. Overall, the analysis found that branded drug companies paid $57.7 billion in rebates to pharmacy benefit managers and health plans in 2015, up from $33.2 billion in 2013. In addition, the companies paid $28.3 billion in rebates under the Medicaid program for the poor, up from $19.1 billion in 2013.
“Much of the media and much of the public discussion is focused on the list price” for drugs, Stephen Ubl, PhRMA’s CEO, said in a telephone interview. “This study is the first to show what happens when list price meets the forces of the private market.”
Pharmacy benefit managers have said their negotiations help keep drug prices in check, in part by pitting rival drugmakers against each other to get better deals.
The report “shows something that we’ve been saying all along: that payers have been demanding and getting bigger and bigger discounts and rebates as drug prices rise,” said Mark Merritt, CEO of the Pharmaceutical Care Management Association, an industry association that represents PBMs.
While individual clients of PBMs can get rebate information, Merritt said that it would undermine competition in the market to publicize detailed information on rebate amounts.
“Gross” Invoice Cost for Top Selling Generic and Brand Prescription Drugs – Volume 151
The costs shared here are what the pharmacy actually pays; not AWP, MAC or WAC. The bottom line; payers must have access to actual acquisition costs or AAC. Apply this knowledge to hold PBMs accountable and lower plan expenditures for stakeholders.
Step #1: Obtain a price list for generic prescription drugs from your broker, TPA, ASO or PBM every month.
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our acquisition costs then determine if a problem exists. When there is a 5% or more price differential (paid versus actual cost) we consider this a problem.
Multiple price differential discoveries means that your organization or client is likely overpaying. REPEAT these steps once per month.
— Tip —
Always include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to determine if better pricing is available in the marketplace compared to what the client is currently receiving.
When better pricing is discovered the contract language should stipulate the client be indemnified. Do not allow the PBM to limit the market check language to a similar size client, benefit design and/or drug utilization. In this case, the market check language is effectually meaningless.
- Go to the previous page
- 1
- …
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- …
- 90
- Go to the next page