Employers would like to see changes spread to the business sector as prescription costs climb [Weekly Roundup]
Employers would like to see changes spread to the business sector as prescription costs climb and other notes from around the interweb:
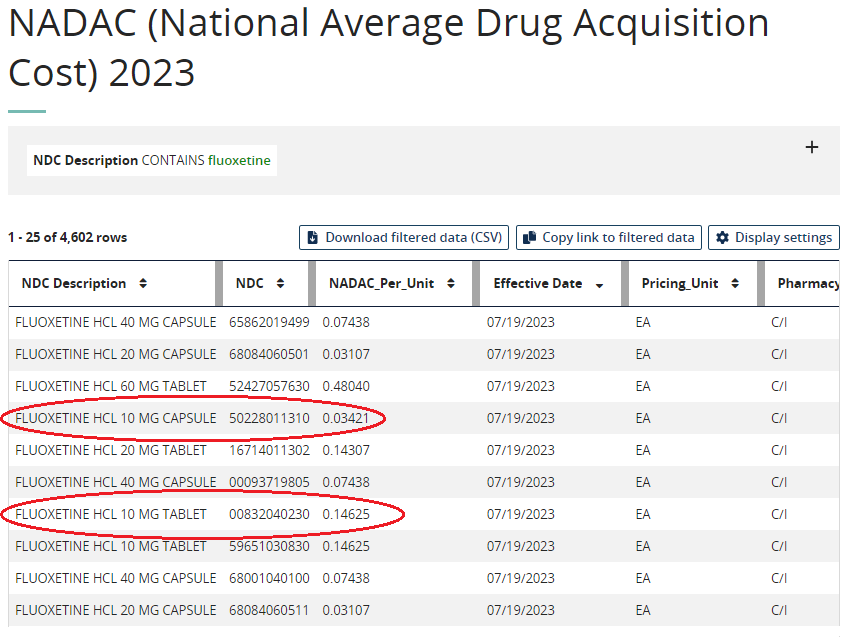
- Employers would like to see changes spread to the business sector as prescription costs climb. The cost of pharmaceuticals is a key topic for policymakers on the Hill, and it should come as no surprise that it’s also a major concern for employers across the country. The Business Group on Health released its annual survey of large employers this week and found that 91% are either concerned or genuinely very concerned about overall pharmacy cost trend. Alongside that finding, the survey identified that the median spending on pharmacy continues to grow, rising from 21% in 2021 to 24% in 2022. In addition, 92% said they were either concerned or very concerned about high-cost drugs coming through the pipeline. Specialty pharmacy accounts for a growing portion of health spend, and orphan drugs for rare, complex diseases account for large swaths of products coming to market.
- DOJ Generic Drug Price-Fixing Settlement. Teva Pharmaceuticals on Monday announced that it reached a deferred prosecution agreement with the U.S. Department of Justice over its drug price-fixing case involving generic drugs. Under the deferred prosecution agreement (DPA), Teva will pay a total of $225 million over a five-year period starting next year. From 2024 to 2027, the company will make $22.5 million tranches, culminating in a $135 million lump sum in 2028. Teva also agreed to divest one additional generic product to a third-party buyer. In return, the DPA will allow Teva to sidestep a mandatory exclusion from U.S. federal healthcare programs, which would have been the company’s punishment if the case had gone to trial, and it had been found guilty. In its news release, Teva pinned the drug price-fixing charges on a single former employee, who between 2013 and 2015 “agreed with competitors that Teva would not bid on an opportunity to supply that customer with a particular generic product.” As part of the agreement, the company has also committed to implementing and maintaining compliance controls to prevent such incidents from happening again.
- Playbook for Employers – Addressing PBM Misalignment. The guide, released by the National Alliance of Healthcare Purchaser Coalitions, identifies several key strategic recommendations that employers can adopt when looking to better navigate their relationship with PBMs. For one, the playbook recommends that employers find advisers that are genuinely putting in the work for them. Advisers should be independent and transparent, according to the guidebook, and contracts should be designed to ensure that PBMs act in the employer’s best interest. “As we uncover these increasingly apparent anomalies, I think we’ve got to challenge ourselves to do better and most importantly require that our advisers, our middlemen and our intermediaries do better on our behalf,” Mike Thompson, CEO of the alliance, told Fierce Healthcare.
- STAT News investigation takes deep dive into PBM broker conflicts of interest. Employers across the country — from big names like Boeing and UPS to local school systems — pay consulting firms to handle a straightforward task with their prescription drug coverage: Get the best deals possible, and make sure the industry’s middlemen, known as pharmacy benefit managers, aren’t ripping them off with unfair contracts. But a largely hidden flow of money between major consulting conglomerates and PBMs compromises that relationship, a STAT investigation shows. Some consulting firms often are getting paid more — a lot more — by the PBMs and health insurance carriers that they are supposed to scrutinize than by companies they are supposed to be looking out for.