Tuesday Tip of the Week: PBMs can be Fiduciaries
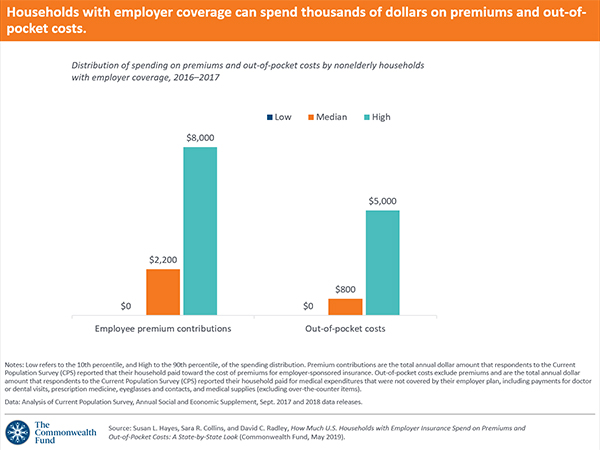
It’s not important to me who is right or wrong. I’m focused on making sure plan sponsors get the right information. Ohio’s Attorney General in 2019 called for PBMs to be fiduciaries. Still there is doubt among commercial and public sector employers, unions, health plans and health systems whether a PBM can act as a fiduciary. Very few purchasers of PBM services are asking for a fiduciary model in their pharmacy benefits management request for proposals, for instance.
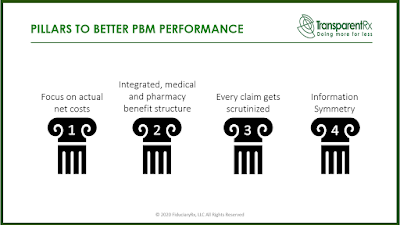
Pass-through and transparent PBM business models don’t inherently eliminate wasteful and duplicative spending. Because these models thrive on optics and not delivering lowest net cost, they can leave plan sponsors mired in the status quo. In their middleman role, PBMs have used secrecy and subterfuge to pad their own profits instead of passing savings along to customers. John Paul Jones wrote, “It seems to be a law of nature, inflexible and inexorable, that those who will not risk cannot win.”
 |
| Click to Learn More |
“When state agencies entered into these nebulous deals with PBMs, they unknowingly hired a fox to guard the henhouse,” Yost said. “But he was a smart fox. He didn’t kill the chickens; he helped himself to the eggs.” The attorney general recommended “a solution based on market principles” identifying four objectives that should be met:
1) State drug purchases should go through a master PBM contract that is administered through a single point of contact.
2) The Ohio Auditor of State should have unrestricted authority to review all PBM drug contracts, purchases and payments.
3) PBMs must be fiduciaries.
4) Nondisclosure agreements (NDAs) on drug pricing with the state must be prohibited.
What was the broker or consultant’s role in that situation? There are situations where you have someone who is trying to prove that they’re valuable by trying to play hardball with people and spin it as if they are looking out for you. On March 15, 2019 AG Yost filed suit against OptumRx on behalf of the Ohio Bureau of Workers’ Compensation seeking to recover nearly $16 million in overcharges to the fund intended to protect injured workers.