An appellate court has determined OptumRx’s bid did not conform to the bid solicitation, because it included language reserving the right to modify the financial terms of the deal to protect its profit if the state made changes to the plan design.
“Optum’s additional language … permitted it to ‘hedge’ its bid, thereby reducing its financial risk from adverse plan design changes,” the court said. “That set it apart from the other bidders who agreed to be bound by all of the terms of the bid solicitation.”
Tyrone’s Commentary:
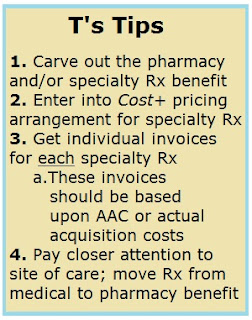
I here it all the time from purchasers of PBM services; control the formulary, go for low net cost, not high rebates, work with a transparent PBM, or make sure the consulting firm isn’t being comped. Everyone knows these things are important, but the execution is usually poor. Furthermore, if the self-insured employer and its consultant aren’t informed or highly sophisticated it can lead to bad contract language that isn’t consistent with bid responses or permits the PBM to modify terms during the contract’s life, for instance. There are three parts to being an adept steward of a pharmacy benefit and they are not mutually exclusive. In other words, if you’re poor in any one of these areas it will hurt you in the other two.
1) Education. If only I had a nickle every time a consultant or HR executive said I don’t need any PBM education. That’s like LeBron James saying I don’t need to practice playing basketball. He’s the best in the world yet he still studies the game more than any other player! You may attend a webinar or two, read a blog post or chat with peers and I can tell you it still isn’t enough to beat non-fiduciary PBMs at their own game. Invest more time and money into becoming a better steward of pharmacy benefits. Incrementalism in this area will not be rewarded. The best proponent of transparency is informed and sophisticated purchasers of PBM services.
2) Procurement. Means the action of obtaining or procuring something. When obtaining PBM services, ideally it involves a reverse auction. The state of New Jersey ran a reverse auction but somehow Optum’s bid still squeeked through. My guess is that human interference got in the way, as it often does, with the real bid winner or the reverse auction was inherently flawed. Because one takes action on a problem doesn’t guarantee an optimal outcome. You can swing (act) at a 95 mph fastball but will miss (outcome) 99 out of a 100 times unless of course you’re a well-trained professional and student of the game. There are a lot of companies and consultants that procure PBM services who are missing a lot! One problem is a lack of accountability unlike standing in the batters box alone. It would be nice if self-insured employers had a stopgap like an appellate court to fall back on. Oh wait they do and they’re called benefits consultants.
3) Vigorous Oversight. PBM performance should be monitored on an ongoing basis far beyond standard reports. The types of routine monitoring activities performed by the plan sponsor can vary based on past performance with the PBM or the nature of the services performed. The type and frequency of monitoring should be documented in the contract before it is executed. The plan sponsor should establish key performance metrics designed to measure PBM services. The PBM oversight program must also define what happens if the vendor’s performance is below the plan sponsor’s performance expectations. When noncompliant performance occurs, the plan sponsor should request a formal action plan defining specific activities to ensure performance meets the defined expectations.
The state, meanwhile, argued Optum’s language was meaningless and didn’t affect the outcome of the auction. The three-person court invalidated the contract, saying its size, complexity and potential savings for the public aren’t a shield from this type of review.
“No savings can justify the impairment to the integrity of the bidding process caused by an irregular proceeding, the court said.
[Read More]